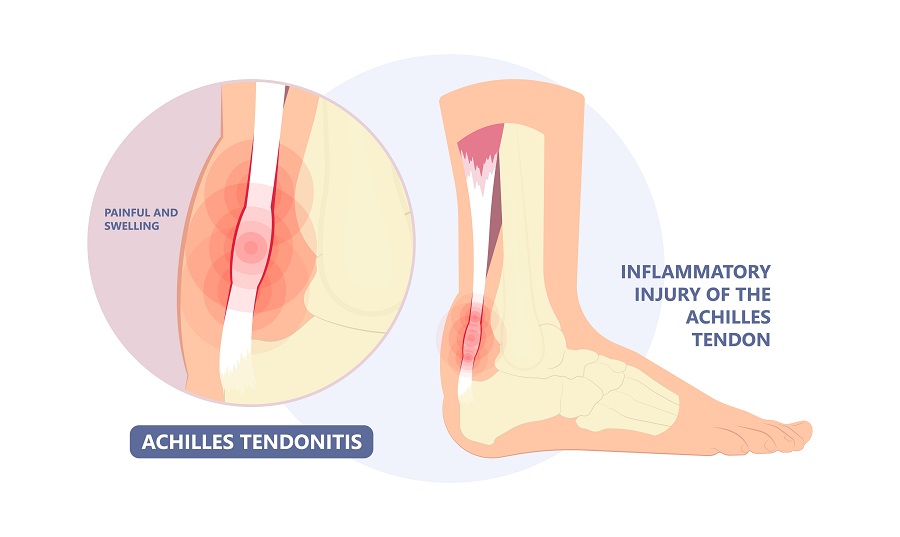
 Big toe joint pain can be one of the most frustrating foot complaints. It is simply because the great toe joint has a very important function for normal walking. Arguably, it is probably one of the most important joints in the foot and ankle. A lot of your body weight rolls over it as your body propels forward. Therefore, any pain or limited range of motion in this joint makes it difficult to engage in activities. You may compensate so much that you will have pain elsewhere such as the heel or Achilles’ tendon. You may also have a lot of pain first thing in the morning when you get up. It may be difficult to wear shoes that have any type of heel because there is more pain when the toe is forced to move up. You may also have a painful enlargement on the top of the joint that causes pain when shoes rub it.
Big toe joint pain can be one of the most frustrating foot complaints. It is simply because the great toe joint has a very important function for normal walking. Arguably, it is probably one of the most important joints in the foot and ankle. A lot of your body weight rolls over it as your body propels forward. Therefore, any pain or limited range of motion in this joint makes it difficult to engage in activities. You may compensate so much that you will have pain elsewhere such as the heel or Achilles’ tendon. You may also have a lot of pain first thing in the morning when you get up. It may be difficult to wear shoes that have any type of heel because there is more pain when the toe is forced to move up. You may also have a painful enlargement on the top of the joint that causes pain when shoes rub it.
Big Toe Joint Basics
Much like the kneecap, the patella, the big toe joint has two sesamoid bones. These bones sit underneath the big toe joint. They are oval-shaped bony structures with muscles and tendons attached to them. They help increase strength so that we have more power to push off the toe. Similar to how the knee cap functions for the knee joint. The big toe joint should have a lot of range of motion, approximately sixty degrees upward off the walking surface. When the joint becomes damaged, and range of motion is reduced significantly pain results along with an altered gait.
Causes for Toe Joint Pain
- Foot type(biomechanics) – For many, it is biomechanics. People can have a foot type that allows them to walk a certain way, and because of their improper foot mechanics, the great toe joint starts to jam. This can take place over many years so by the time you reach middle age the range of motion in the joint could be dramatically reduced. Along with this, there can be a spur on the top of the great toe that will make the knuckle look exceptionally large. The name commonly used to describe this condition is Hallux rigidus or Hallux limitus. Both describe that the Hallux (big toe) has limited motion. What is going on inside is that joint cartilage is starting to wear down because of this jamming effect. Therefore, you are getting the degenerative joint disease (osteoarthritis) along with this. Understand that just because you are getting osteoarthritis in the toe does not mean you’re going to get it in other joints because this common condition is based upon foot mechanics.
- Sesamoiditis – You may also find that you have pain not throughout the joint, but rather just on the bottom of the big toe. This could very easily be caused by irritation to the sesamoid bones. This can happen from damage to the sesamoid bones. This could be from excessive weight-bearing beneath the big toe for long periods or from trauma. Or with an injury, the sesamoid bones could be fractured.
- Trauma – Trauma can also cause pain in the great toe joint. It could be trauma from the toe getting jammed, and therefore cartilage inside the joint is damaged and this could result in long-term pain that eventually leads to more long-term arthritis because the cartilage has now been damaged. As I mentioned before, you can also get sesamoid pain from trauma to the great toe joint.
- Arthritis – Patients can have rheumatoid arthritis or psoriatic arthritis that’s caused by autoimmune disease. This can also affect a great toe joint. This is usually also going to affect other joints in the hands and the feet.
- Gout – The big toe is commonly affected by gout. The toe will become very warm and red. Gout can be very painful. It is commonly treated by certain types of nonsteroidal anti-inflammatory or medication to lower uric acid in the blood which when elevated puts you at risk for gout.
Treatments for Toe Joint Pain
Treatments can vary from simply using medication such as anti-inflammatory medication, different shoe gear, possibly orthotic devices in the shoe gear, or surgery. First, let us talk about shoe gear. If you find that your toe doesn’t want to move very much, you may need to consider a shoe that doesn’t flex as much. Stiff-soled shoes are sometimes helpful. If you’re a lady, you must avoid heels. If you find that you have a knuckle on the top of the toe that’s sticking up, you also may need to avoid a shoe that rubs against this knuckle area, as this could also cause pain. If you have pain underneath the big toe, as we spoke about before with sesamoiditis pain, you may find that you need to wear a shoe that has quite a bit of support or some cushioning underneath the great toe, so that you’re not impacting the sesamoid bones as much.
Medication
Whether you have just generalized wear and tear on the great toe joint, which we call hallux limitus or hallux rigidus, or if you have a more complicated issue with an autoimmune disease like rheumatoid arthritis, oftentimes anti-inflammatory drugs or special drugs for an autoimmune disease may be prescribed.
It’s my opinion that long-term use of anti-inflammatory drugs, such as ibuprofen are not good for the health of the joint and should be used sparingly. However, if you are suffering from an autoimmune disease such as rheumatoid arthritis following your doctor’s recommended medication is important advice.
Orthotic Devices
Orthotics are especially useful to help with the reduction of the progression of hallux limitus, and also with the pain, especially in the early phases of hallux limits. You will also find that orthotics are excellent for the treatment of sesamoid pain underneath the big toe joint. If your shoes are not helping enough you need to consider orthotic devices.
Regenerative Therapeutics
Delaying or avoiding surgery!! Currently, as we’ve been using regenerative therapeutics for many years for problems such as plantar fasciitis and Achilles tendon pain it’s also been useful to eliminate joint pain not only in the great toe and ankle but other joints of the foot. We originally started with PRP( platelet enriched plasma) and more currently use umbilical cord or placenta cell products. This technique has been extremely useful to delay or avoid surgical treatments.
Surgery
Surgery for hallux limitus could be as involved as a fusion of the great toe joint or the use of an artificial great toe joint. But in most cases, the surgery that is used is simply to remove the spurring on the top of the great toe that is causing the jamming; and in some cases, repositioning the joint will help it move more freely. These can be quite successful.
In conclusion, if you have great toe joint pain, don’t put up with it for long. It is a very difficult problem to live with – especially if you’re always having to favor your great toe joint or find it difficult to wear certain shoes. It’s best to treat it early because the measures that we take at Anderson Podiatry Center are proactive and we will do our best to avoid surgery for your toe joint pain.



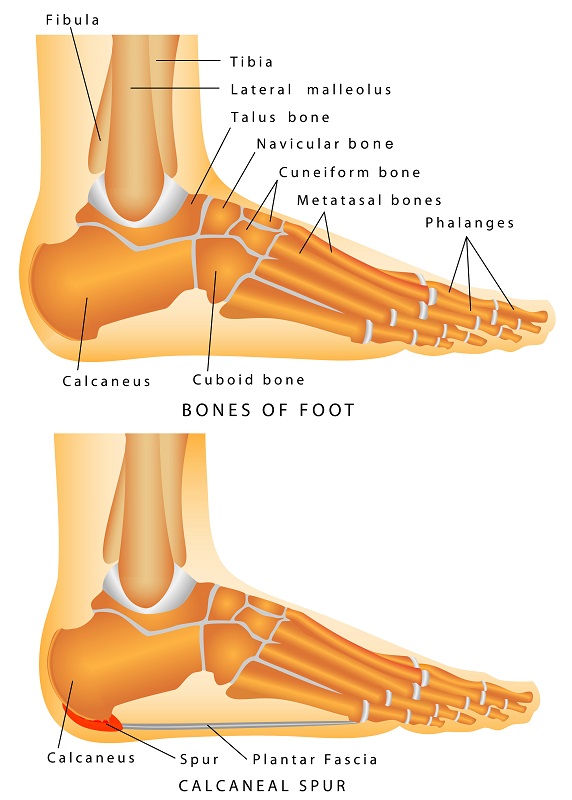 Let’s start with the basics. Many of you have heard of plantar fasciitis. The plantar fascia is a strong fibrous band of tissue that runs along the bottom of your foot starting in the ball and attaching to the bottom of the heel. With every step you take as the arch flattens the fascia is being pulled. When you are a teenager or child its very flexible like a rubber band but as you get older it loses its elasticity and starts to pull from where it attaches to the heel. So, let’s discuss the actual heel spur. Many patients will have a heel spur on the bottom of the heel on x-ray. This is a calcium deposit that may occur from the constant pulling of the fascia on the heel in this location. It is a bony protrusion that extends from the heel bone towards the toes. Another theory is that there can be microfractures in the heel from the fascia pulling so hard and the spur in a result of the heel bone attempting to repair. So, the most current understanding is that the actual spur is seldom if ever the true source of your pain. It is the result of the fascia pulling from the bone. What is the evidence to support this?
Let’s start with the basics. Many of you have heard of plantar fasciitis. The plantar fascia is a strong fibrous band of tissue that runs along the bottom of your foot starting in the ball and attaching to the bottom of the heel. With every step you take as the arch flattens the fascia is being pulled. When you are a teenager or child its very flexible like a rubber band but as you get older it loses its elasticity and starts to pull from where it attaches to the heel. So, let’s discuss the actual heel spur. Many patients will have a heel spur on the bottom of the heel on x-ray. This is a calcium deposit that may occur from the constant pulling of the fascia on the heel in this location. It is a bony protrusion that extends from the heel bone towards the toes. Another theory is that there can be microfractures in the heel from the fascia pulling so hard and the spur in a result of the heel bone attempting to repair. So, the most current understanding is that the actual spur is seldom if ever the true source of your pain. It is the result of the fascia pulling from the bone. What is the evidence to support this?










 What exactly is an ingrown toenail?
What exactly is an ingrown toenail?