Julie was giving up her golf game . Her heel hurt so bad she had to be rescued by a golf cart. We discussed her treatment options with the goal of getting rid of the pain that was ruining her life and avoiding heel surgery. Please watch to learn more. If you’d like more information about how we can help eliminate your heel pain using our advanced technologies please go to our website.
Author: admin
Heel and Arch Pain: Revealing the Seven Steps to Take
Heel and arch pain can be persistent and painful. The runs and walks you once enjoyed can become a thing of the past; you may start to gain weight, and it can even impede your sleep. The start of the day can be met with extreme pain as you first step down on that heel. It generally affects people physically and mentally.

Considering the function that our feet have, it’s amazing how well they work since they are required to:
- Balance the entire body
- Adapt to irregularities in terrain
- Maintain our balance as we stand
- Take on more pressure when we gain weight
- Help our body change directions
- Function as a shock absorber
Due to these responsibilities, there are a multitude of problems that can cause heel and arch pain.
Plantar Fasciitis
Plantar fasciitis, commonly referred to as heel spur pain, tends to be worse early in the morning when you first stand up. You may find yourself hobbling to the bathroom, but after you’re going about for a few minutes, the pain may to dissipate and get better as the day progresses. This is caused by the fascia, which runs from the ball of your foot to your heel – it often tends to get overstressed therefore causing the tight band of tissue to pull or tear away from the heel. The pain affects directly under the heel where you are bearing weight. Although it is commonly referred to as plantar fasciitis, more recent studies support that it’s not inflamed but rather broken down. So, a term you may hear more of in the future is plantar fasciosis which more accurately describes the condition. It is also now understood that the heel spur you may see on X-ray does not cause the pain, but it is rather the fascia pulling from the same area on the heel bone.
Posterior Tibial Tendonitis
The posterior tibial tendon is a tendon that attaches into the arch of the foot. It’s a very important tendon for stabilizing the foot. If the foot tends to overpronate, which we call flattening, then this tendon can be overworked and this can also frequently cause pain. Particularly, as you get older, the tendon starts to wear down.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome can also occur. This may cause burning and tingling and numbness in the arch. It’s less common, but can also be causing pain in the arch.
Arch Pain
If the pain is through the arch it may be from muscle or ligamentous fatigue. This may be caused by a foot that flattens (pronates) over a very high arch which is called a cavus foot.
What causes these problems?
- Obesity
- Overuse of the arch
- Improper and run down shoes
What you can do?
- Use ice and rest the area.
- Purchase over the counter anti-inflammatories.
- Choose over the counter inserts for more support.
- Modify your activity by temporarily switching to biking rather than running.
- Reduce going barefoot as much as you can. Wearing shoes can offer more support and can reduce pain.
- Stretch your calf muscle. If your calf muscle is tight, your ankle can’t flex. It puts more pull and strain on the plantar fascia and other tissues in the arch.
- Evaluate your shoes. If they don’t support you enough, you might be due for a new pair.
When should you seek professional help?
If you’ve tried the suggested home remedies and the pain is persisting and/or getting worse, seek medical attention from a foot specialist. It should also be stressed that if you think you injured your foot (either you fell, landed wrong, heard something pop or have significant swelling) seek medical attention immediately.
What is required of you?
- A good medical history – Oftentimes your story will tell the doctor the diagnosis.
- A physical exam- a lot can be learned from the examination. This can tell the doctor whether the pain is localized or from an overstrained plantar fascia or a tight calf muscle.
- Other tests that may be done
- X-rays
- Diagnostic Ultrasound
- MRI
What are the treatments the doctor may discuss with you?
- Use of custom-made orthotics to give more precise support to the foot
- Cortisone injections
- Physical therapy
- Immobilization with a cam boot
- Stretching and possible use of night splints
- Stem cell – regenerative medicine treatment
- Laser treatments
If the conservative measures fail and significant heel and arch pain remains, the option of surgery may also be discussed. In the case of plantar fasciitis, conservative measures are usually successful, so rarely does a situation occur where surgery is necessary, but if it is, it is highly successful when performed.
What Are the Benefits of Wearing Orthotics?
As a podiatrist, we often recommend orthotic devices as they can be of great benefit for the wearer. Before we dive into the benefits of wearing orthotics, let’s answer the question of what an orthotic is, from a podiatrist point of view.

In today’s world, it seems like everyone is marketing their orthotics. You see them in retail stores, shoe stores, ski shops, and even Facebook ads. As a podiatrist, the whole concept of what an orthotic is has been muddied. My opinion is shared by my colleagues- podiatrists believe there is a non-weight-bearing, neutral-point position of the foot. And so, whatever technique is utilized to fabricate an orthotic, an impression of the foot should be taken in this position.
The foot is positioned at its optimal functional position. Any kind of orthotic that is made from a technique that involves any partial or full weight-bearing, we feel is not done accurately. There are small, torsional abnormalities, sometimes between the front half and rear foot, that are not taken into account when the foot is bearing weight. A podiatrist’s orthotic is much more precise and is able to support and control excessive motion in the foot more accurately. That is not to say that an orthotic made from a weight bearing technique won’t work, but the chances are greatly reduced. It is a common story of patients we treat.
Benefits of Orthotics
I am writing this blog at a time where some advocate barefoot running, or running in minimalist shoes. So hear me out from a foot specialist’s point of view. Outside the office, when someone finds out I’m a podiatrist, I’m often asked what types of shoes are best. Using tact, I’ll make the point that it’s like asking an optometrist what lens prescription they should have. We expect that kind of precision for our eyes, but medicine seems to not think the same rules apply to the feet.
If one has excellent foot structure, I’m not opposed to the idea of barefoot running. My point is that it all starts with what foot type you’ve inherited. It has been observed that 70% of people may have feet that overpronate. Pronation is simply the motion that involves the flattening of your feet. The foot will flatten the arch and abduct, or move away from the other foot. A more ideal foot type does not overpronate, and the actual bony structure helps stabilize and support the foot. There is a locking mechanism that takes place in the bones in the midfoot area. Those that have feet that are much more flexible, or pronates more easily, are thought to have a foot where the bones do not lock and support the foot. Therefore, soft tissue needs to. This can cause excessive stress on structures such as tendons, joints, nerves and other soft tissue structures such as fascia. So, how do you know if custom orthotics might be useful? The following are some tips and specific conditions you should know about.
If you keep getting the same type of injury or foot pain over and over, or if you’ve had that injury for an extended period of time, it may be time to look into orthotics. Especially if you’ve already tried resting, anti-inflammatories, and icing the area. This could also be an indication that your foot type lends itself towards having specific issues.
Soft tissue problems
- Plantar fasciitis and Achilles tendinitis
- One of the more common problems is plantar fasciitis commonly referred to as heel pain. Orthotics will reduce the stress of the plantar fascia pulling on the bottom of the heel. For Achilles tendonitis the stress on the Achilles will be reduced.
- Foot deformities
Nerve problems
- Neuromas and tarsal tunnel syndrome
- Neuromas are a nerve enlargement that can occur in the ball of the foot. If you’re experiencing burning, tingling and numbness on the bottom of your foot, you may have tarsal tunnel syndrome.
- Joint pain
- Arthritis in the foot can also be treated with orthotics and it’s a safer, drug free approach. This may include big toe joint pain commonly referred to as Hallux limitus. Also, ankle pain and pain in the small joints in your arch.
Final Thoughts
- You may save money as you’ll quit shopping for shoes to solve your foot problems. The orthotic can be taken from shoe to shoe and will neutralize the less optimal shoe as it’s designed precisely for your foot.
- You’ll avoid injuries as certain foot structures lend themselves to certain injuries
- You could lose weight and sleep better as you become more active.
If you yourself frustrated with your inability to stay active, please consider a consultation with us to truly understand more about the foot structure you have and how it may be the issue that no one has explained to you. There are many benefits of wearing orthotics, so it’s time you discover for yourself!
Are Custom Orthotics For Foot Problems Right For You?
There are two basic principles to consider when dealing with your feet and your lower extremity pains that you may have. First, do you think you have a foot that over flattens, otherwise called pronation? As foot specialists, we have been trained in biomechanics and believe that most patients are born with different foot types. If you tend to overpronate the bony structure of your foot, you cannot adequately support the foot. This results in soft tissue structures being stressed more. Orthotics simply position the foot so that the joints can support the foot and demand less of other structures.
 Secondly, do you have a condition that continues to plague you in spite of attempts with anti-inflammatories, icing, resting or maybe even physical therapy? Do you find that if you lay off from running or walking and return to it, the same problem occurs? If this is you, then this blog is right for you! Let’s find out if custom orthotics for foot problems are right for you.
Secondly, do you have a condition that continues to plague you in spite of attempts with anti-inflammatories, icing, resting or maybe even physical therapy? Do you find that if you lay off from running or walking and return to it, the same problem occurs? If this is you, then this blog is right for you! Let’s find out if custom orthotics for foot problems are right for you.
Over-pronation
Let’s address your first concern. Over pronating is a very simple concept to understand. People tend to flatten their arch or roll their foot inward too much and too often. The old adage is, if you walk in the sand and you can’t see much of an arch, this could be an indication of pronation. This is somewhat true in most cases, but it may be more complex than that. Some people have an arch that doesn’t over flatten; but if you look at their heel from behind, their heel tends to roll in quite a bit. It does not stay perpendicular to the ground.
Different kinds of feet present different kinds of pronation. Sometimes, a professional is the best to tell you if you are an overpronator. If you have tried various treatments and you have had a problem that’s been persisting; for over one, three, six or twelve months – it is an indication that your foot structure needs additional support. The following are some conditions that are oftentimes bettered or totally eliminated with the use of orthotic devices.
Achilles Tendonitis and Plantar Fasciitis
Pain on the bottom of the heel is referred to as plantar fasciitis. It’s one of the most common problems to be treatable. Tendon on the backside of your heel or running up the Achilles tendon, is, oftentimes, Achilles tendonitis. Orthotics can treat this a great deal. In many cases, treatment options such as anti-inflammatory stretching and physical therapy just don’t knock it away.
Bunions and Foot Deformities That Are Treated With Custom Orthotics
Bunions are a prime example of this, especially if it’s in early stages and not painful yet. There is a chance of a foot deformity where you can feel growth on the back of your heel; also called the Haglund’s deformity or pump bump. Patients can benefit from orthotics in this situation. In both cases, the biomechanics of your foot might allow you to have a progression of a bunion or progression of the bump on the back of heel.
Stiff Toe Joint
Also referred to as hallux limitus or hallux rigidus, this is an arthritic condition in its early stages and can be healed with orthotic devices.
Painful Ankle
The ankle in itself can have arthritis and orthotics may benefit that. There are stabilizers or stirrup tendons that help stabilize the outer side and the inner side of the ankle. If you have overpronation, these tendons tend to have to be overused because they’re trying to stabilize the foot that is unstable.
Knee Pain
Orthotics have a proven track record of helping what is called chondromalacia patella, which occurs when the kneecap is not centered over the knee joint, thereby causing arthritis between the knee joint and the femur bone. There are instances when people have a higher Q-angle and their knee angulates inward so the thigh and lower leg are not in a straight line. By supporting the foot more this can lessen the angulation at the knee with every step that is taken. The patella can then stay in better alignment and may be less likely to wear down the cartilage. If you have any of the above conditions or just simply have a problem that persists for a long time, orthotics may be just the way to go for you.
Finally if you find yourself in pain in the ball of your foot maybe you’re feeling like your sock is wrinkled but it isn’t. You may be suffering from a nerve enlargement called a neuroma (mortens neuroma) . Orthotics can help as they support the area to lessen the rubbing of a ligament against the nerve.
This blog will serve as a guideline for your consideration of custom orthotics for foot problems and what they are useful for. Depending on your condition, orthotics may be a part of the solution or the only treatment that is needed. So remember to consider if you think you’re an overpronator and are having difficulty getting rid of a chronic problem in the foot or ankle.
What You Should Know About Bunion Treatment
What Are Bunions?
You have all seen a person wearing beautiful sandals, but notice a big bump or protrusion on the side of their foot by the big toe. Or maybe you’ve seen an area of the shoe by the big toe that is being pushed out- looking as though it wants to bust through. This is a bunion.
 There are several hereditary factors that can cause bunions; and the most popular opinion is that shoes aggravate it. Bunions become a big issue when they start to cause skin irritation, redness and swelling, so it’s fair to look into bunion treatment options before things get bad.
There are several hereditary factors that can cause bunions; and the most popular opinion is that shoes aggravate it. Bunions become a big issue when they start to cause skin irritation, redness and swelling, so it’s fair to look into bunion treatment options before things get bad.
Why Do We Get Bunions?
There are varied factors that lead to the formation of bunions. As foot specialists, we believe that in most cases shoes can aggravate the problem, but are not usually the main cause. In fact, the foot type you’ve inherited has a lot to do with creating the bunion.
The first metatarsal (the bone that leads down to the great toe joint) needs to be very stable. Many people tend to over-flatten their feet in their arch, causing instability of the first metatarsal. This results in an abnormal pulling of the tendons which causes the big metatarsal to move away from the others, thus creating the bunion bump. To simplify, the bump is caused by the misalignment of the first metatarsal and the second metatarsal.
There are other bunion formation theories that involve the shape of the tarsal bones (these are the small cube-shaped bones in your arch). Some believe that the different shapes of these bones associated with your first metatarsal leads to more instability, and therefore can create the bunion deformity angle.
Treatment:
There are various bunion treatments that can be attempted, such as padding, wearing different shoes, custom-made orthotics or cortisone injections. Oftentimes these can help, especially if the bunion is at an earlier stage, but in many cases these options are only a temporary fix.
It is important to know that as time goes on and the deformity of the bunion gets worse, people can even develop an arthritic condition in the great toe joint.
For many patients, surgery is the most popular bunion treatment option because it is considered a permanent correction. We discuss this very carefully with patients because it can lead to risks such as recurrence, infection, nerve injury, or slow/delayed bone healing.
The Most Popular Surgical Options:
There are different approaches taken to correct a bunion surgically – the simplest being what is called the Silver bunionectomy (also known as the McBride bunionectomy). This involves shaving off the extra bone on the inside of the big toe. Another common procedure is the Austin Bunionectomy, where the bone by the big toe joint is pricesely shifted over towards the second bone; therefore reducing the angle between the two bones.
Depending on the severity of the deformity, other bunion treatment options may take precedence – such as the removal of a wedge of bone towards the arch. This is reserved for more severe deformities and will also close the angle down to bring the first metatarsal closer to the second metatarsal.
At Anderson Podiatry Center, we believe we have perfected these techniques to give our patients the maximum correction, so they can get back to normal activity in their shoe gear. For most patients, it takes six to eight weeks to achieve this. If you’ve started noticing difficulty in wearing shoes, and are therefore limiting your shoe selection, please book an appointment to discuss treatment options. A consultation with us can go a long way; let us help you get back to pain-free activities.
Does Chronic Pain Affect Your Personality?
The term chronic pain syndrome is used quite a bit nowadays since so many people experience it. In many cases, people even end up with drug addictions because of it. Here, we will discuss what qualifies as chronic pain and the various ways it affects you physically and mentally.
 What is Chronic Pain?
What is Chronic Pain?
The most common notion is that chronic pain is caused from nerve damage, possibly by trauma or from surgery. You may be in a car accident and suffer whiplash or a fractured ankle, and right after your surgery to repair the fracture chronic pain will ensue. The trauma of surgery or an injury can trigger chronic pain. This may be surprising, but something as simple as an ankle sprain may create a state of chronic pain.
The medical terms you may have heard for these conditions are Complex Regional Pain Syndrome, abbreviated as CRPS, and Reflex Sympathetic Dystrophy, abbreviated as RSD. RSD was the term used to describe the pain patients thought they were consigned to and had to learn to live with. In 1993, the terminology was changed to CRPS, Complex Regional Pain Syndrome, but some still will use the original terminology. When you hear that someone is going to a pain clinic for treatment, this is most commonly what they have been diagnosed with.
Neuropathy and Restless Legs Syndrome
Problems such as neuropathy and restless legs syndrome can also be included in the chronic pain group. The symptoms of neuropathy can include burning, tingling, numbness, and pain, and is more common in the lower extremity than the upper. Neuropathy is often associated with diabetes, but can also be called idiopathic neuropathy, meaning it’s from an unknown cause. Restless legs syndrome can also be considered a chronic pain problem when it is severe. The symptoms associated with it are a nervous or restless type feeling in the legs that makes it difficult to sit still. Sufferers are often awoken by this feeling in the night and must get out of bed to relieve the symptoms. Other symptoms include a creepy crawly sensation, cramping and jerking in the legs. All these symptoms make it difficult to have uninterrupted sleep and ultimately affect your personality.
 Chronic Pain and Your Personality
Chronic Pain and Your Personality
With chronic pain syndrome, the body goes into a fight or flight mode. This changes the chemistry within the brain; creating emotional issues where people want to isolate themselves – all resulting in depression. When a great part of your time is spent thinking about and focusing on your pain it can become very difficult to focus on other things or people. This feeling of isolation can lead to a depressive state.
Chronic pain can also cause significant anxiety – the feeling of hopelessness that a problem may never get resolved. Patients may also feel a loss of control, not knowing what to do and are desperate for help or improvement. In this case of restless leg syndrome, there can be severe sleep deprivation which also causes depression and anxiety in the inevitable terrible night of bad sleep.
A study reports that people with chronic pain may tend to worry more, which causes them to be less inclined to participate in novel activities. The desire of wanting to go out and explore the world goes away, ultimately minimizing the pleasures of life.
There’s also evidence that chronic pain can cause an alteration of how communication between brain cells takes place, thereby reducing your ability to effectively process your own human emotions. Without the ability to monitor your emotions, people experience a lack of control or misinterpretation of what is happening. The main way to treat this problem is to find the cause of the issue.
Weight Gain and Depression
Weight gain that comes with lack of activity and lack of sleep can also cause personality changes. When sleeping becomes difficult and your focus is on your chronic pain, it reduces one’s self-esteem. The combination of lack of sleep, the emotional stress of the pain and potential side effects of the medication taken for these disorders make it difficult to get up each day, let alone be active.
This lack of activity can commonly lead to weight gain. Why is this so important? We know that lack of exercise has a negative effect on the biochemistry of your brain, and the potential for weight gain can also have an effect on one’s self esteem. The relationship between one’s physical and mental self is very important, and if you are not being greeted by the great looking self you once saw yourself as you can experience hardship.
At Anderson Podiatry we provide many options, including working with peripheral nerve disorders, that can get to the root of these problems rather than treating the symptoms with medications. We like to describe this method as “putting out the fire” rather than simply dealing with the smoke. So, if you’re questioning if you have mood or personality disorders from your chronic pain, please come visit us. Do not lose hope as we’ve been able to help many get back to feeling like themselves.
How to Avoid a Visit to the Doctor’s Office When Experiencing Heel Pain

One of the most common foot complaints is heel pain, which is commonly referred to as Plantar Fasciitis. Here we’ll discuss how to prevent a visit to the doctors office when experiencing heel pain and what you can do at home to help alleviate your symptoms.
The symptoms of heel pain often start at the bottom of your heel and are very prevalent when first getting up in the morning. This is a very common complaint, and even though the pain can gradually get better throughout the day, it’s important this is treated right away. When plantar fasciitis pain is mild, you have a better chance of reversing the pain with some simple recommendations.
Shoes and Orthotics
First and foremost, the most important thing to do is to make sure your shoes are not run down. Shoes eventually wear down and do not give the foot as much support as they used to, which can cause pain. If you’re an active runner or a walker, good shoe support is key. If you are flatfooted, this becomes even more significant. 
With every step you take the foot flattens, causing the fascia to pull from your heel, which can cause symptoms of heel pain. So, utilizing more support in the shoe can be very beneficial. If you don’t believe your shoes are worn down, another option would be to buy over-the-counter shoe inserts, which are also known as orthotics.
There are many options when purchasing orthotics, and you can typically find them in an athletics store. However, be careful when going to an orthotics outlet because oftentimes these devices can cost several hundreds of dollars- and you’re better off seeing a podiatrist to have custom orthotics made to work for your foot type. Ideally, you should not be spending more than $10-$15 for store-bought inserts.
Icing the area of heel pain from plantar fasciitis
Icing is often used to treat sports medicine injuries and can also be employed for the reduction of pain and inflammation caused by heel pain. If you do choose to ice the area, it’s important to do it for 10 minutes twice a day. You can also roll your heel on a frozen plastic bottle as this can be beneficial.
Stretching
Stretching before you get up in the morning can also help as it can reduce the pain and inflammation of the plantar fascia. In order to stretch this area correctly you should keep your knee straight and put your foot up towards you. By keeping your knee straight you are stretching your calf and achilles tendon; this will allow your ankle to flex up more and thereby lessen the need for excessive pulling of the fascia. The band of tissue you can feel beneath your skin in the arch is the fascia. It is often suggested to be careful with this because there have been cases where this can actually worsen the symptoms.
Another way to help stretch the achilles, calf and plantar fascia is by using a night splint. Although they have shown to be useful for many, they can also be an annoyance and reduce sleep quality.
Anti-Inflammatories for heel pain from plantar fasciitis
Anti-inflammatories can also be taken. These medications help with the pain and inflammation for those experiencing mild plantar fasciitis. Anti-inflammatories can be taken for approximately one or two weeks to see if they help.
Cut Down on Activities
Lastly, it’s important to back off your activity level. While moving around may be a part of what you do, it’s not helping your heel heal! You can back off entirely, or even cut it down by 50%. One of the most common causes of heel pain is doing too much too soon. When people take up a new form of exercise, such as walking or running, it is important to factor in days of rest- especially since your body requires long periods of rest when injured. Resting is as important as the stress you put on your body to become more fit. Therefore, if you’re walking or running five days a week, maybe cut back to just two or three to see if there is improvement.
If you’ve attempted these treatments for heel pain from plantar fasciitis approximately three to four weeks and have seen no results, it’s probably time to consider professional attention as you may need more aggressive treatment options. Even so, it is important to note that early and aggressive intervention can spare you a trip to the podiatrist’s office.
Our Revolutionary Approach to Restless Leg Syndrome Treatment

The name “restless legs syndrome” does not do the severe nature of the condition justice as it has been said that 10% of the population suffers from restless legs; and out of those, half have it severely. Restless leg syndrome is also known as Willis-Ekbom disease and is twice as common in female patients. Here at Anderson Podiatry, we have a revolutionary approach to the treatment of restless leg syndrome and are eager to share our findings with you.
Symptoms of Restless Legs Syndrome
The symptoms of restless leg syndrome almost always occur at night or at rest, making it difficult for those suffering to fly on a plane or sit in a movie theater. That’s the frustrating thing about restless legs; during the day you may be functioning just fine; but once it’s time to go to bed, it all starts up again. Day after day, the same symptoms occur. At first, it may be mild, but then it can become more severe until it’s consistently happening every night.
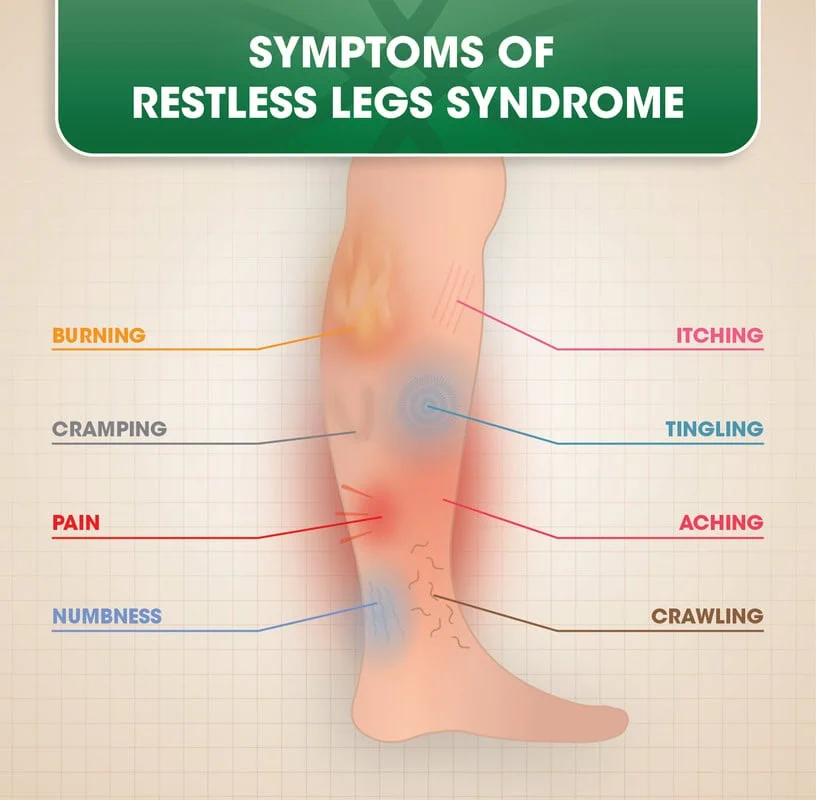 Symptoms are experienced in the legs; particularly from the knee down rather than above. The symptoms can be a combination of cramping, a creepy crawly sensation- like bugs or ants are going on your skin, pain, or jerky legs. However, the most prevalent symptom is an anxious or nervous feeling that makes you want to get up and walk. In fact, most patients have said this is what they have to do during the night.Restless leg syndrome comes on quite slow, and because of this, patients do not realize the severity of the condition. In fact, many in healthcare do not even realize the severity, and their hands are tied because, in many cases, they’re not sure how to help.
Symptoms are experienced in the legs; particularly from the knee down rather than above. The symptoms can be a combination of cramping, a creepy crawly sensation- like bugs or ants are going on your skin, pain, or jerky legs. However, the most prevalent symptom is an anxious or nervous feeling that makes you want to get up and walk. In fact, most patients have said this is what they have to do during the night.Restless leg syndrome comes on quite slow, and because of this, patients do not realize the severity of the condition. In fact, many in healthcare do not even realize the severity, and their hands are tied because, in many cases, they’re not sure how to help.
Aside from all the physical symptoms, maybe the worst of them all is the psychological effect. This includes the anxiety people experience during the day- not wanting to think about what’s going to happen when they go to bed at night- to the anxiety of being up at night when everybody else in the world seems to be sleeping. Then comes the morning and you are absolutely exhausted.
The good news is, for many of you, you can come out of the bushes because at Anderson Podiatry, we understand how severe this is. In fact, we actually have a solution for many people suffering from restless leg syndrome. This is something we’ve been practicing for approximately seven years.
The Conventional Approach to Treatment of Restless Legs Syndrome
In conventional medicine there’s no known cause for restless leg syndrome, so people are often left helpless. In many cases, people also find that their doctors or loved ones do not understand the severity of the problem. This is incredibly unfortunate because restless leg syndrome is a very serious problem that can affect people’s general health. Recent studies have shown that there’s a higher incidence of early death with people experiencing severe restless legs due to lack of sleep. This lack of sleep can cause all sorts of secondary problems, such as increased incidence of diabetes, cancer, and heart disease.
In the world of conventional medicine, the treatment options are very minimal. They usually involve pharmaceutical medications that deal with dopamine levels in your brain, or band-aiding the pain with medications that are used for treatment of neuropathy (namely Lyrica and gabapentin). Outside of this realm of drugs is the possibility that some of your restless legs could be caused by your back. Maybe you have a pinched nerve in your back that could be radiating symptoms in the leg.
So basically, the restless leg syndrome treatment options are relegated to two things; either it’s coming from the back, or in the vast majority of cases, it’s something the medical community does not know how to treat. However, many of these treatments, especially the drugs, can have detrimental side effects patients don’t like, including significant weight gain.
Our Concept
At Anderson Podiatry we prefer to call this disorder “restless legs compression syndrome” because we’ve been able to reverse the symptoms by opening up tight nerve pathways in the lower extremity. When the nerve tunnels become tight it can be damaging, which results in restless legs syndrome symptoms for many. For most, the success rate is incredibly high and there is minimal chance of worsening the condition. We also treat patients with restless leg syndrome non-surgically by utilizing laser and e-stim. Both of these treatments help to restore more normal nerve function and have proven very effective. However, for many patients with severe restless legs, the surgical option may be the best treatment of choice.
So you may be wondering, what do we do when we do surgery? We’re basically opening up nerve tunnels- usually three, but sometimes just two. Two of these nerve tunnels are in the lower leg just below the knee, and third is down in the front of the lower one-third of the leg. These tunnels can create a lot of pressure on the nerves in the legs. Instead of treating you with pharmaceuticals, or hoping that maybe treatment of the back will help, we have found that the fire is truly in the nerve tunnels of the lower extremity. While many treatment options simply blow away smoke from the fire, we believe that we’re able to get rid of the problem by directing our attention to the flames.
Many people are desperate for a solution, and our method of treatment is something you’re not going to hear conventional medicine speaking to. Why? Well, in many cases, it’s because big pharma has no interest in supporting what we’re doing, as it would be contrary to what they want you to think (that restless leg syndrome patients have to be on medication).
In conclusion, if you’re looking to target the direct cause of your problem, consider coming to our office for evaluation of restless leg syndrome treatment. For many, surgery may not be the option you desire, and this is a decision that we can mutually discuss. If you have any other further questions, please contact our office to get a better understanding of how our treatment options work. It’s time for you to get your life and sleep back.
Please visit our YouTube channel, where we have plenty of information about what we do, as well as testimonials from patients that have successfully gone through our surgical procedures and nonsurgical treatment options.
COVID-19 Update
Now Offering Telemedicine and Home Visits!
Click Here for Dr. Anderson’s Video Message On COVID-19

An update on COVID-19 from Anderson Podiatry Center and Anderson Podiatry Center:
We are closely monitoring events in our local community and continuously updating our policies and protocols as new information arrives.
Please know that during the stay in place order, we are a Designated Essential Business so we are available to consult with most patients in need, and we adhere to best practices for hygiene, infection control and medical professional team health. We are screening patients for symptoms and possible exposure before they enter our office for any urgent or needed ongoing care. We are also offering telemedicine and home visits to reduce social interaction. Read abou tinformation on how the vaccine may affect you in our blog on nerve damage.
For any questions or for foot, ankle or chronic pain problems you are experiencing. We’ll get you taken care of!
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.
The End Of Heel Pain! Our 1-2…..-3 Punch Treatment!
(Be sure to watch until the end of the video for an Ultrasound visual of before and after Ray’s fascia!)
Ray’s bump in the trail.
The plantar fascia has a BIG job. It stabilizes the arch of the foot and allows flexion of the first metatarsal, enabling the first metatarsal to carry the majority of the body weight. In other words, when the plantar fascia gets tired and aggravated, you’ll know very quickly! Your heel will hurt like crazy, especially if you’re an active person like our patient, Ray. “Before I came to see Dr. Anderson for treatment, I had heel pain for about a year. I would get this pain when I would run, or hike or snowshoe… so a lot of things that I enjoy doing!”
Running out of options…
“After about 9 months of this, I couldn’t run… I couldn’t do any of these things that I enjoyed.” Ray attempted physical therapy for relief, but with no avail. While we were impressed with Ray’s perseverance, we were very eager to ease him of his heel pain. After meeting with Ray, we found that he actually had Plantar Fasciosis, which means that his fascia was deteriorating rather than getting inflamed! Knowing this offered Ray the ability to get treatment specifically tailored to the ACTUAL cause.
Our 3 Step Approach!
“So I went to Dr. Anderson, who gave me custom orthotics, laser therapy, and regenerative medicine.” We ended up taking Ray through our 3 step approach for heel pain from start to finish! At Anderson Podiatry Center, our ultimate goal is to ensure we can get our patients back to the activities they enjoy as fast as possible. Ray was in a hurry to get back into action, and as exercise enthusiasts ourselves, we understood his urgency! We took him through these 3 steps so that he could get back out on the trail as quickly as possible.
It’s a RUNderful life!
“3 months after having the injection, orthotics and the laser therapy, I feel 100% better! I can run, I can hike, I can do anything that I want. Now I’m back to running 10-15 miles a week!”
Our doctors deeply care about our patients and their recovery, even well after we treat them. We always follow up with our patients, and after a recent follow up with Ray we were ecstatic to hear that he recently ran 9 miles without any heel pain! He was excited to announce that he is currently training for a half marathon.
If you or a loved one have been putting the activities that make you happy on the backburner! We would love to get to know you, hear about what’s been holding you back, and work with you to plan an approach to rid you of heel pain!






