Diabetes is becoming more common worldwide. It is known that the number of people with diabetes is soaring. Countries where diabetes used to be rare such as China are seeing a significant increase. Why is that? Many experts would agree it’s the increase in spread of the American diet worldwide which can cause obesity ,one of many risk factors. It is thought that 22 percent of patients with diabetes in the United States are undiagnosed.
What are the symptoms of prediabetic neuropathy?
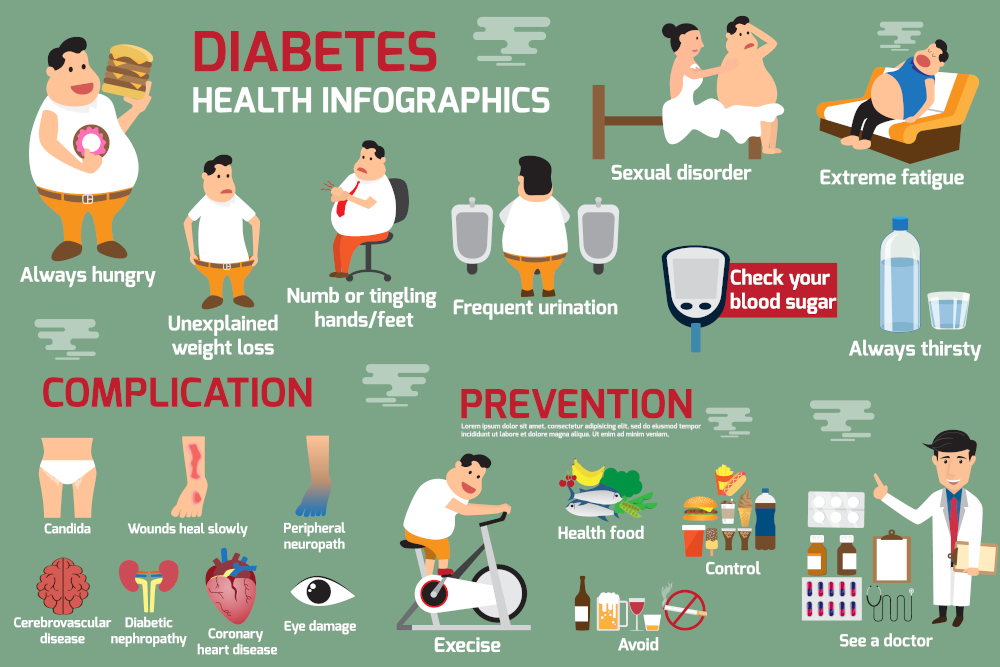
Neuropathic pain can include burning, tingling and numbness and in more severe cases muscle weakness may also occur. These symptoms occur in the feet and are called peripheral neuropathy. When your glucose levels increase your nerve fibers are damaged. This can lead to Type II diabetes and nerve damage.
How do I know if I’m becoming a diabetic?
The two most common blood studies done are glucose fasting and Hemoglobin A1C. Glucose fasting is taken after you fast and most laboratories will consider anything over 100 abnormal. Hemoglobin A1c will let you know over a period of the last two to three months has your glucose levels have been in an abnormal range. Anything under 5.7 is considered normal with the borderline range going from 5.7-6.4 so anything over 6.4 will be considered diabetic.
Is there a better way to know if you are becoming diabetic?
Yes, there is and the answer lies in two additional tests called insulin fasting and glucose tolerance testing. They can be the leading indicators that you’re progressing towards being prediabetic and having neuropathy symptoms.
Fasting insulin– this test measures your insulin level which will be elevated if you’re prediabetic. This lab result should be low. Under 5 is ideal and when it starts to be elevated to 10 or higher it and indication your prediabetic. When you have high insulin levels its an indicator that you’re attempting to get glucose out to the blood and into the body’s tissues. This can be from a high intake of sugars and carbohydrates.
Glucose tolerance test– This is a test taken after you have fasted. You drink a solution of sugar and the sugar levels are measured one hour after the intake. If you are normal, the glucose levels will elevate but to a reasonable level. If you are prediabetic the sugar levels will be excessively elevated. It’s telling you that you have impaired glucose tolerance meaning you’re becoming insulin resistant. The pancreas is no longer able to create enough insulin and therefore the body’s tissues become unable to respond to the effect of insulin which is to deliver glucose from the bloodstream to the body’s tissues. Therefore, your blood sugars levels are elevated.
These two tests are used infrequently. From personal experience, I find many patients with the beginnings of neuropathy type symptoms will report to me that they have had borderline Hemoglobin A1c for 2,3 or 4 years. This is a frequent occurrence for those of us trained in peripheral nerve surgery. Once Hemoglobin A1c levels get into the abnormal range patients are placed on medication. It’s my opinion this is by design. It’s this doctors concern that Big Pharma has managed to educate doctors that this is how the rules are played. Unfortunately, what some podiatrists see are patients who are developing neuropathy and never had their insulin levels or glucose tolerance tests done. Sadly these test results may have indicated that they are heading towards a diabetic state.
Armed with this information, the patient would have the option to exercise more or modify their diet to either delay or avoid the diabetic state.
What complications can arise from prediabetic neuropathy in the foot?
Complications can include suffering from the symptoms of neuropathy which can interfere with your activities and sometimes makes sleeping difficult. But most importantly complications can include amputations.
Three things you can do to reverse this issue.
- Exercise – This does not have to be complicated, just find something you enjoy doing and be consistent with it . Walking 20-30 minutes three times a week alone can help. Lifting weights , swimming, or pickleball.
- Modify your diet – avoid as many processed foods as possible. Some of these may be loaded with different types of sugar that you may not be aware of. Many have high levels of fructose corn syrup which may be the worst form of sugar; many juices also contain this.
- Reduce your intake of sugar and carbohydrates.
- Consider eating more fats – Healthy fats in meat and even bacon if it is grass fed are helpful as these fats satiate your appetite and you’ll eat less. Use more grass-fed butter and consider using it in your coffee.
- Consider intermittent fasting – start by fasting 12 hours and eventually build up to 24 hours. You might be surprised at how much more energy you have and it lets your digestive system rest. This includes your pancreas where insulin is created.
Prevention of Prediabetic Neuropathy
Preventing prediabetic neuropathy involves a proactive approach to maintaining stable blood sugar levels and leading a healthy lifestyle. Making small, sustainable changes can significantly delay or even avoid the onset of neuropathy symptoms. Here are a few additional strategies to consider:
- Regular Check-Ups: Routine medical screenings can help catch early warning signs of prediabetes. In addition to blood sugar and A1c tests, discuss adding insulin fasting and glucose tolerance tests with your healthcare provider if you are at risk. Early detection can give you the chance to make meaningful changes before neuropathy becomes an issue.
- Focus on Weight Management: Studies show that maintaining a healthy weight is one of the most effective ways to prevent insulin resistance and manage blood sugar levels. Combining a balanced diet with regular physical activity can keep your weight in check and help prevent the progression of diabetes.
By adopting these preventive steps and being mindful of lifestyle habits, individuals can reduce their risk of developing prediabetic neuropathy and related complications.
So if you think you have prediabetic neuropathy, please consider asking for all four tests that we spoke about in this blog. It may give you the advantage of being proactive and avoid being placed on medication. You can visit our locations in Fort Collins Podiatrist in Fort Collins, Colorado and Broomfield, Colorado.


 The diagnosis is made simply by the symptoms that you have. There is no test that is done to diagnose Restless Legs Syndrome. However, some doctors may have sleep studies done to confirm that you have jumpy legs. There are multiple symptoms that collectively cause uncomfortable sensations in your legs. One of the most common is the irresistible urge to move the legs. This will be noticed when you’re sitting or lying down. This is relieved when you get up and move. Other symptoms can include:
The diagnosis is made simply by the symptoms that you have. There is no test that is done to diagnose Restless Legs Syndrome. However, some doctors may have sleep studies done to confirm that you have jumpy legs. There are multiple symptoms that collectively cause uncomfortable sensations in your legs. One of the most common is the irresistible urge to move the legs. This will be noticed when you’re sitting or lying down. This is relieved when you get up and move. Other symptoms can include:





 Stretching for sever’s disease can be important in the early stages, as it is thought that the soft tissues that attach to the heel may become too tight. The Achilles tendon has two muscles that attach to it. One muscle group is called the gastrocnemius muscle and its origin is above the knee joint on the femur bone. Its primary function is to lift the heel off the ground and propel the body forward while running or walking. The other muscle is the soleus. This muscle is a stabilizer and helps support the ankle joint while standing. The soleus originates below the knee. The anatomy of these muscles is important to understand so that stretching is done properly.
Stretching for sever’s disease can be important in the early stages, as it is thought that the soft tissues that attach to the heel may become too tight. The Achilles tendon has two muscles that attach to it. One muscle group is called the gastrocnemius muscle and its origin is above the knee joint on the femur bone. Its primary function is to lift the heel off the ground and propel the body forward while running or walking. The other muscle is the soleus. This muscle is a stabilizer and helps support the ankle joint while standing. The soleus originates below the knee. The anatomy of these muscles is important to understand so that stretching is done properly.