Have you heard these comments regarding peripheral neuropathy?
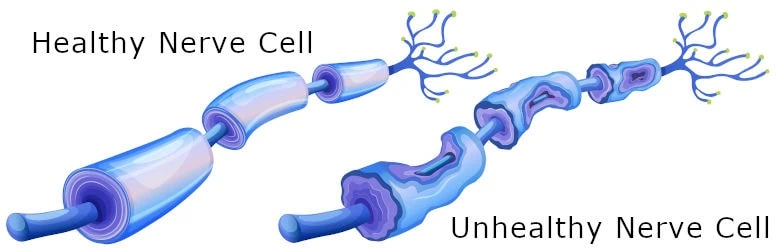
“The nerve fibers have disintegrated so they are permanently damaged, it’s irreversible.” “There is no cure.” Listening to this, you walk away from whichever doctor told you this and you say to yourself “Oh well, I guess the nerve damage is permanent and there is nothing I can do to change that.” Typically, if your neuropathy is severe, you may walk away from this healthcare encounter with a prescription of Lyrica, Gabapentin, or a Narcotic. In this blog we talk about your treatment options and the different stages of peripheral neuropathy.
Challenging what conventional medicine is telling you because it is false! It’s not true!
Aside from treatments aimed at reducing carbohydrate and sugar intake in your diet or looking at vitamin deficiencies; current medical treatment involves two options, however, there is a third option that very few of you hear about.
Option 1 -The problem is metabolic.
It may be from diabetes or if one is prediabetic. It could be from an autoimmune disease, alcoholism, thyroid condition, or an unknown cause. Therefore, the nerves are damaged and just don’t work well.
Option 2 – The problem starts in the back.
So the back needs to be addressed. Maybe, you see a chiropractor, get injections in your back, go through surgery on your back, or use nerve stimulators or pain pumps in your back.
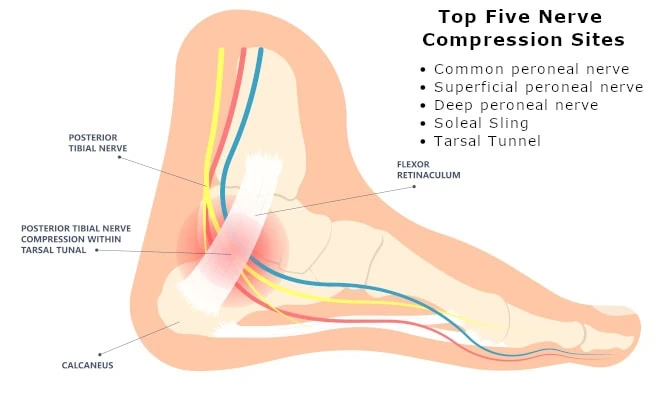
Option 3 – The problem is mechanical and it is in the foot and legs.
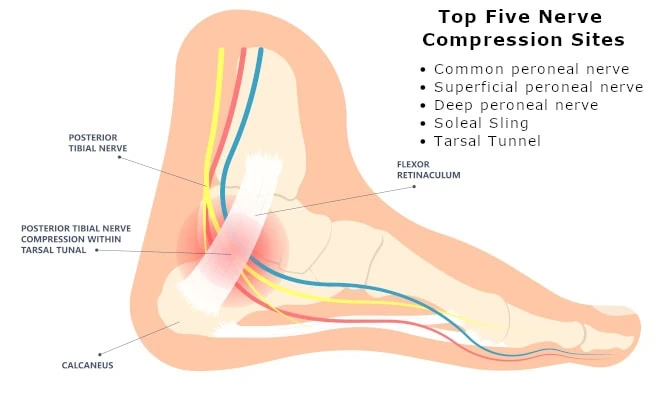
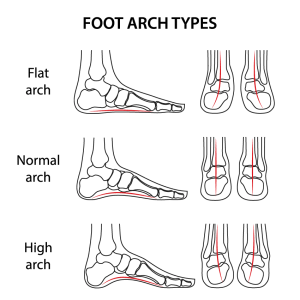
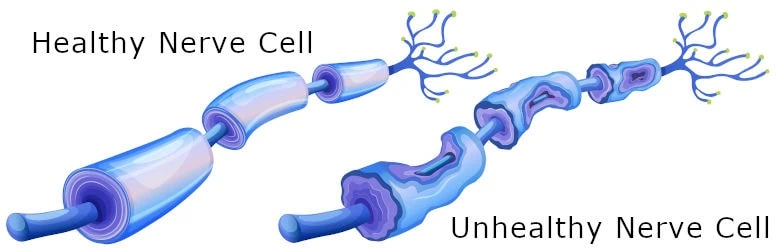
To understand this option, we must look elsewhere at the upper extremities, hands, and arms. When burning, tingling and numbness occur, doctors are trained to consider nerve tunnels such as the carpel tunnel. They are looking for a mechanical problem. Could there be a tight nerve tunnel that is compressing the nerve, and if so surgery to open the nerve tunnel would be considered. This may occur in both diabetic and non-diabetic neuropathy. Our research provides objective evidence of this. (Ref, Anderson 1, Yamasaki 2) The nerves can be damaged from metabolic processes but there’s another solution to fix the problem. Very few doctors have been trained to evaluate and treat nerve pathways in the lower extremities. So, surgical treatment must be considered in the five stages to save lives and limbs, especially when one has a diabetic condition. It may even have a positive effect on blood vessels. In the diabetic state, it is known that because of high sugar levels, the body produces a sugar by-product called sorbitol. This sugar will reside in the nerve tissue and will attract water to the nerve causing swelling. Now with a larger nerve, the nerve tunnels that the nerve branches pass through become tighter. (Ref D Lee; D Dauphinée, J. Jakobsen 3, J. Jakobsen 4. With this information in mind, it is ideal to consider surgical decompression to relieve pressure on the nerve.
So here are the stages of peripheral neuropathy and what to do
First Stage – In this stage of peripheral neuropathy, the symptoms of burning tingling, and numbness may be very inconsistent and sporadic. The intensity of the burning, tingling, and numbness in the feet or the legs comes and goes. At this stage, looking at the possibility of being prediabetic is important, and nutritional modifications may have a significant impact
Second Stage – The symptoms will now be getting more intense and frequent. Patients are more concerned and may be more likely to seek treatments. At this stage, nutrition considerations are still useful and consultation with a peripheral nerve specialist should be considered to address surgical or non-surgical options.
Third Stage – This is when the symptoms will peak. At this stage, the symptoms may be 24/7 and it may become difficult to sleep comfortably, and walking may be more difficult because of the pain. Many patients may consider medication such as Gabapentin or Lyrica or even pain medication or narcotics. At this stage, nutritional options will have less impact and the option for surgical decompression should be considered. When symptoms are the worst, surgery may be more impactful.
Fourth Stage – In this stage, the severity of the pain and burning may decrease, and walking may now be affected by numbness and weakness. With balance and reflexes being affected, concerns about using a cane or walker are common. In diabetics, the risk of an amputation starts to go up. At this stage, nutritional options do not help that much, and surgical options may still be considered. Now the risk of amputation in the diabetic becomes more real.
Fifth Stage – At the final stage, the nerve is very damaged and there is little pain. The feet will be number and weaker. Walking becomes more challenging and in diabetics, the risk of amputation is more common. This is the stage of peripheral neuropathy where amputations are most likely to occur. Surgery may still be entertained, but it may not be as effective as if it had been performed in stage three or four.
In summary, consider the following when dealing with different stages peripheral neuropathy
Get treatment early to know if you have neuropathy in early stages one and two. Addressing it nutritionally may also have more impact. For most types of neuropathies, you should be evaluated for nerve compression by stages two or three. Especially in diabetics, at the stage where you’re contemplating medication, nerve decompression surgery should be considered. Rather than being medicated through the most painful stages of peripheral neuropathy, patients may want to consider the surgical option of treatment to maximize potential reversal of nerve damage. Waiting till stages four or five may limit the potential improvement gained by surgical decompression. By addressing stages two and three the potential to avoid amputation, limb loss, and possible death could be reduced in diabetics. In summary, as more patients are learning about nerve compression in the lower extremity, the health risks can be eliminated especially in those suffering from diabetic neuropathy.
- Anderson JC, Nickerson DS, Tracy BL, Paxton RJ, Yamasaki DS. Acute Improvement in Intraoperative EMG Following Common Fibular Nerve Decompression in Patients with Symptomatic Diabetic Sensorimotor Peripheral Neuropathy: 1. EMG Results. J Neurol Surg A Cent Eur Neurosurg. 2017 Sep;78(5):419-430. doi: 10.1055/s-0036-1593958. Epub 2016 Dec 30. PMID: 28038479. https://pubmed.ncbi.nlm.nih.gov/28038479/
- Yamasaki DS, Nickerson DS, Anderson JC. Acute Improvement in Intraoperative EMG During Common Fibular Nerve Decompression in Patients with Symptomatic Diabetic Sensorimotor Peripheral Neuropathy: EMG and Clinical Attribute Interrelations. J Neurol Surg A Cent Eur Neurosurg. 2020 Nov;81(6):484-494. doi: 10.1055/s-0040-1701619. Epub 2020 May 26. PMID: 32455446. https://pubmed.ncbi.nlm.nih.gov/32455446/
- Lee, D., & Dauphinée Damien M. (2005, September 1). Morphological and functional changes in the diabetic peripheral nerve using diagnostic ultrasound and neurosensory testing to select candidates for nerve decompression. Journal of the American Podiatric Medical Association. https://meridian.allenpress.com/japma/article-abstract/95/5/433/156230/Morphological-and-Functional-Changes-in-the
- Jakobsen, J. (1978, February 1). Peripheral nerves in early experimental diabetes – diabetologia. SpringerLink. https://link.springer.com/article/10.1007/BF01263449
Frequently Asked Questions (FAQs) About Stages of Peripheral Neuropathy
- What is neuropathy and what are its symptoms?
Neuropathy, also known as peripheral neuropathy, involves damage or dysfunction of the peripheral nerves, leading to symptoms like numbness, tingling, burning sensations, and pain typically in the hands and feet.
- What causes neuropathy?
Various factors can cause neuropathy including diabetes, chemotherapy, certain infections, and physical injuries. Each type has its own specific causes and risk factors.
- Are there different types of neuropathy?
Yes, there are more than 100 types of peripheral neuropathy, each characterized by the specific nerve types involved and the symptoms presented.
- How is neuropathy treated?
While there is no cure for neuropathy, treatments are available that focus on managing symptoms and underlying conditions. These can include medications, physical therapy, and in certain cases, surgical options like nerve decompression surgery.
- What are the long-term impacts of neuropathy?
Neuropathy can be a chronic condition with symptoms that vary in severity. Long-term impacts might include persistent pain, increased sensitivity to touch, and potential mobility issues due to muscle weakness or coordination problems.




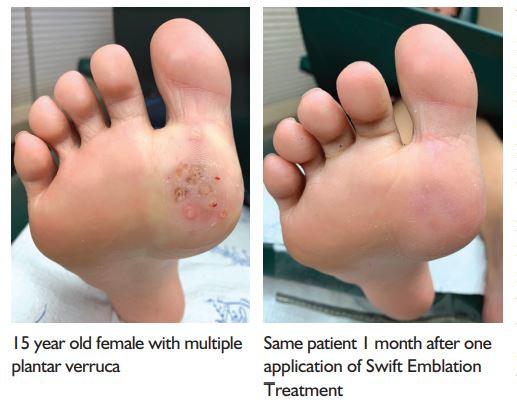 Soft tissue foot reconstructive surgeries may include treatment for ganglions and fibromas. Ganglions can originate from a tendon sheath or from joint capsule. In some cases, the doctor may be able to aspirate the fluid out with a needle in an office setting but if the problem returns or the ganglion is large surgical excision may be the treatment of choice. This can help with the pain and cosmetically improve the look of the foot or ankle.
Soft tissue foot reconstructive surgeries may include treatment for ganglions and fibromas. Ganglions can originate from a tendon sheath or from joint capsule. In some cases, the doctor may be able to aspirate the fluid out with a needle in an office setting but if the problem returns or the ganglion is large surgical excision may be the treatment of choice. This can help with the pain and cosmetically improve the look of the foot or ankle.










 Opiate Addiction
Opiate Addiction