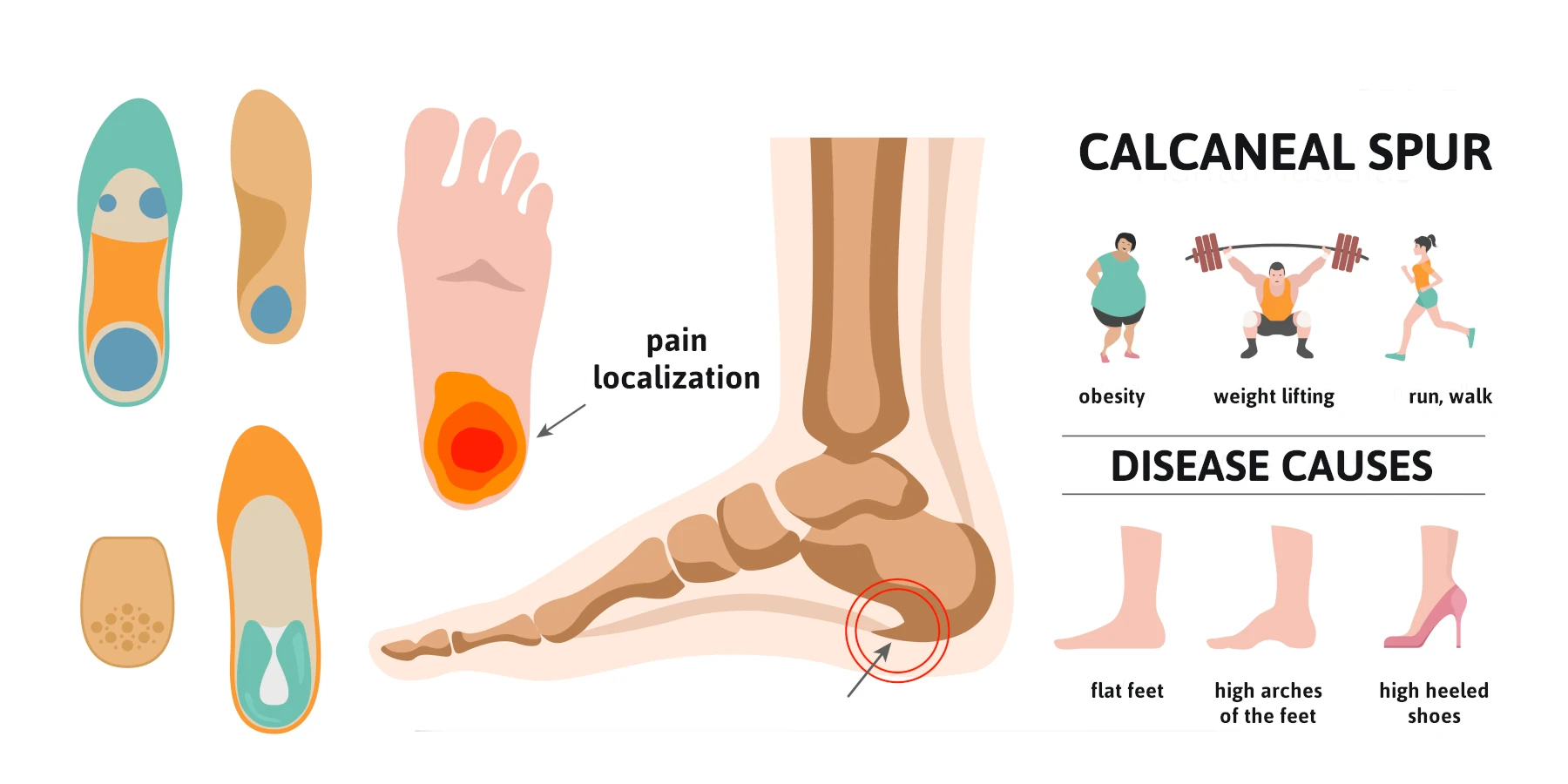
A calcaneal spur, often referred to as a heel spur, is a bony growth that develops on the heel bone (calcaneus). This condition is commonly associated with plantar fasciitis, which involves inflammation of the plantar fascia ligament, leading to significant heel pain. While many individuals manage heel pain through conservative treatments, some may require calcaneal spur surgery to alleviate persistent discomfort and restore mobility. This blog aims to provide a better understanding of why the removal of the heel spur is rarely needed and can be considered a fallacy. I will contrast the old-school ideas with the more recent concepts based on science.
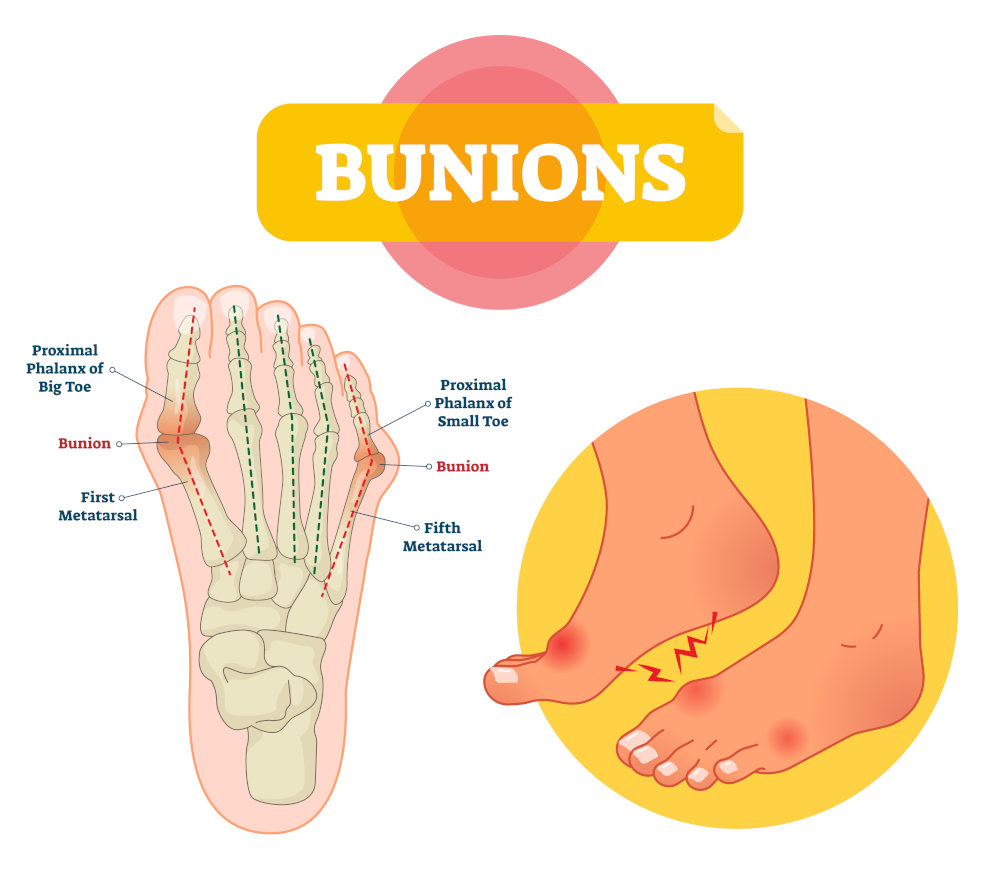
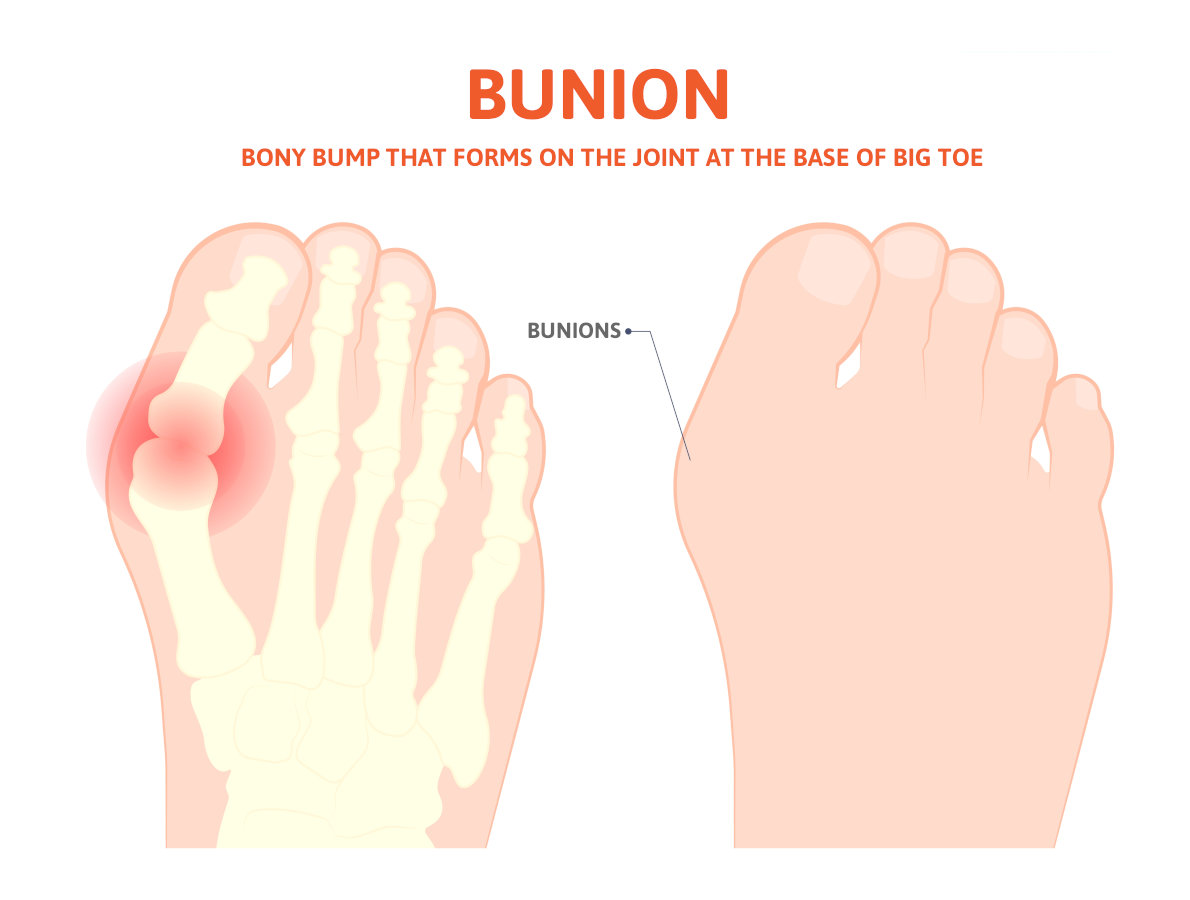
What is a Calcaneal Spur?
A calcaneal bone spur is a bony growth that forms on the underside of the heel bone, typically at the site where the plantar fascia attaches to the calcaneus. Most believe that the point of the fascia from the heel bone at this location may stimulate new bone to form, thus causing the spur formation. In the 1930s, Dr. Spitz was the first doctor to suggest that the actual heel spur is not causing the pain, but rather the fascia that is pulling from the calcaneus.
This condition can arise due to repetitive stress and strain on the foot, often resulting from activities such as running, walking, or standing for long periods. The bone spur development can occur alongside plantar fasciitis, leading to significant heel pain and discomfort. Symptoms may include sharp pain in the heel, especially in the morning or after prolonged periods of sitting. While many individuals experience relief through non-surgical interventions, some may require surgery when conservative treatments fail to provide adequate relief.
Causes of Calcaneal Spurs
Calcaneal spurs commonly develop due to a combination of factors, including:
- Repetitive Stress: Activities that involve excessive strain on the feet, such as running, dancing, or standing for extended periods, can lead to the formation of a heel spur.
- Plantar Fasciitis vs Plantar Fasciosis: the old school concept is that the fascia is inflamed. This has been disproven by one study performed by Dr. Harvey Lamont. When he performed surgery to release the plantar fascia from the heel bone, specimens were sent to a lab. Out of 50 specimens, 49 showed fascial degeneration while only one showed inflammation. This supports that it is not an inflammatory condition.
- Chronic pulling of the plantar fascia can contribute to the development of a calcaneal spur, as the body attempts to stabilize the area by forming new bone.
- Foot Structure: Abnormalities in foot structure, such as flat feet or high arches, can increase the risk of developing heel spurs.
- Age and Weight: Excess body weight can contribute to higher stress levels on the feet.
Symptoms of Calcaneal Spurs
Individuals with a calcaneal spur often experience a range of symptoms, including:
- Heel Pain: The most common symptom is a sharp, stabbing pain in the heel, especially during the first steps in the morning or after prolonged sitting.
- Swelling and Inflammation: The area around the heel may become swollen and tender to the touch due to inflammation.
- Pain with Activity: Activities like walking, running, or standing for long periods can exacerbate heel pain.
- Difficulty in Movement: In severe cases, individuals may find it challenging to walk or engage in physical activities due to discomfort. Understanding these symptoms is crucial for individuals to seek appropriate medical evaluation and treatment.
Diagnosis of Calcaneal Spurs
Diagnosing a calcaneal spur typically involves a thorough evaluation by a healthcare professional. The diagnostic process may include:
- Medical History: The doctor will inquire about the patient’s symptoms, pain levels, and any previous foot injuries or conditions.
- Physical Examination: A physical examination of the foot will help assess tenderness, swelling, and range of motion.
- Imaging Tests: X-rays are often used to confirm the presence of a calcaneal spur and assess its size and location. In some cases, MRI or ultrasound may be utilized to evaluate soft tissue involvement, such as the plantar fascia and the Achilles tendon. An accurate diagnosis is essential for determining the most appropriate treatment options, whether conservative or surgical.
Non-Surgical Treatment Options
Before considering surgery, healthcare providers typically recommend conservative treatment options for calcaneal spurs, including:
- Rest and Activity Modification: Reducing high-impact activities and allowing the foot to heal can alleviate symptoms.
- Physical Therapy: A physical therapist can design a personalized program that includes stretching and strengthening exercises for the foot and ankle, improving flexibility and reducing pain.
- Orthotic Devices: Custom orthotics or shoe inserts can provide additional support and cushioning to the foot, helping to redistribute pressure away from the heel.
- Pain Medication: Over-the-counter medications, such as ibuprofen or acetaminophen, can help manage pain and inflammation.
- Cortisone injection vs Regenerative medicine: Corticosteroid injections may be helpful but rarely provide permanent relief and this is because the fascia is not inflamed, but rather degenerating based upon studies. Therefore, the option of regenerative medicine provides a very success rate to reverse the symptoms on a long-term basis as this treatment helps repair the fascia that is degenerating.
When is Surgery Necessary?
Surgery for calcaneal spurs is generally considered when conservative treatments fail to alleviate pain and improve mobility after several months. Indications for surgery may include:
- Persistent Pain: Severe, ongoing heel pain that significantly affects daily activities and quality of life.
- Diagnosis Confirmation: Confirmation of a calcaneal spur through imaging tests and persistent symptoms despite conservative management.
- Functional Limitations: Difficulty participating in work, recreational activities, or exercise due to heel pain. Surgical intervention aims to remove the spur and address any accompanying issues, such as plantar fasciitis, to restore function and reduce pain.
- Regenerative Medicine: The option of regenerative medicine has greatly reduced the need for surgery. (see testimonial videos)
The Surgical Procedures for a Calcaneal Spur
Contrasting heel spur surgery to endoscopic plantar surgery. Calcaneal heel spur surgery usually involves incision on the side of the heel and the spur is removed along with the attachment of the fascia to the heel bone at the spur location. This is a procedure that surgeons have not performed since 1990. Because the heel spur is not thought to be the cause of your pain, using a small incision to place a scope across the bottom of the heel allows the surgeon to cut a portion of the fascia so that it may stretch and elongate and reduce its pull on the heel bone. This technique has been adopted by majority of the Podiatric Foot and Ankle Surgeons, and because of its high success rates, it supports that fact that the heel spur is not the cause of your pain.
Recovery from heel spur surgery
This type of surgery usually involves a larger incision and more trauma and longer recovery with immobilization in a cast, and sometimes non-weight bearing.
Recovery from endoscopic heel surgery
This type of surgery uses a small incision, and you can bear weight immediately and may return to wearing shoes in 3-4 weeks.
Watch Patient Testimonial Videos
Post-surgery, patients are typically advised to avoid weight-bearing activities for a specified period to allow for proper healing. Physical therapy may be recommended to facilitate full recovery and regain strength and range of motion.
Recovery and Rehabilitation for Calcaneal Spur Surgery
The recovery time for calcaneal spur surgery varies among individuals, with most patients experiencing significant improvement within a few weeks. A typical recovery process includes:
- Pain Management: Pain may be managed with prescribed medications and the application of ice to reduce swelling.
- Physical Therapy: Engaging in physical therapy is crucial for restoring strength, flexibility, and balance. Therapists may focus on exercises to improve range of motion and stability, particularly around the Achilles tendon and plantar fascia.
- Gradual Return to Activity: Patients are typically encouraged to gradually return to normal activities as healing progresses, following their surgeon’s recommendations.
- Long-Term Management: Maintaining a healthy weight, wearing appropriate footwear, and incorporating regular stretching and strengthening exercises can help prevent future heel issues.
Conclusion
Calcaneal spur surgery can provide significant relief for individuals suffering from persistent heel pain due to calcaneal spurs. While many patients find success with conservative treatments, surgery remains an effective option for those who do not respond to traditional methods. Understanding the causes, symptoms, and treatment options for calcaneal spurs is essential for making informed decisions about care. If you suspect you have a calcaneal spur or are experiencing persistent heel pain, consult with a healthcare professional to explore the best treatment options for your needs.