Living with diabetes brings many challenges, and diabetic nerve pain in feet ranks among the most debilitating complications. This condition, called diabetic neuropathy, affects millions of people with diabetes worldwide. The good news is that recent advances in treatment offer new hope for managing this painful condition.
Understanding Diabetic Neuropathy
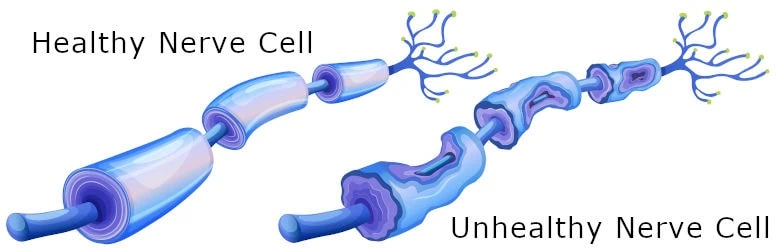
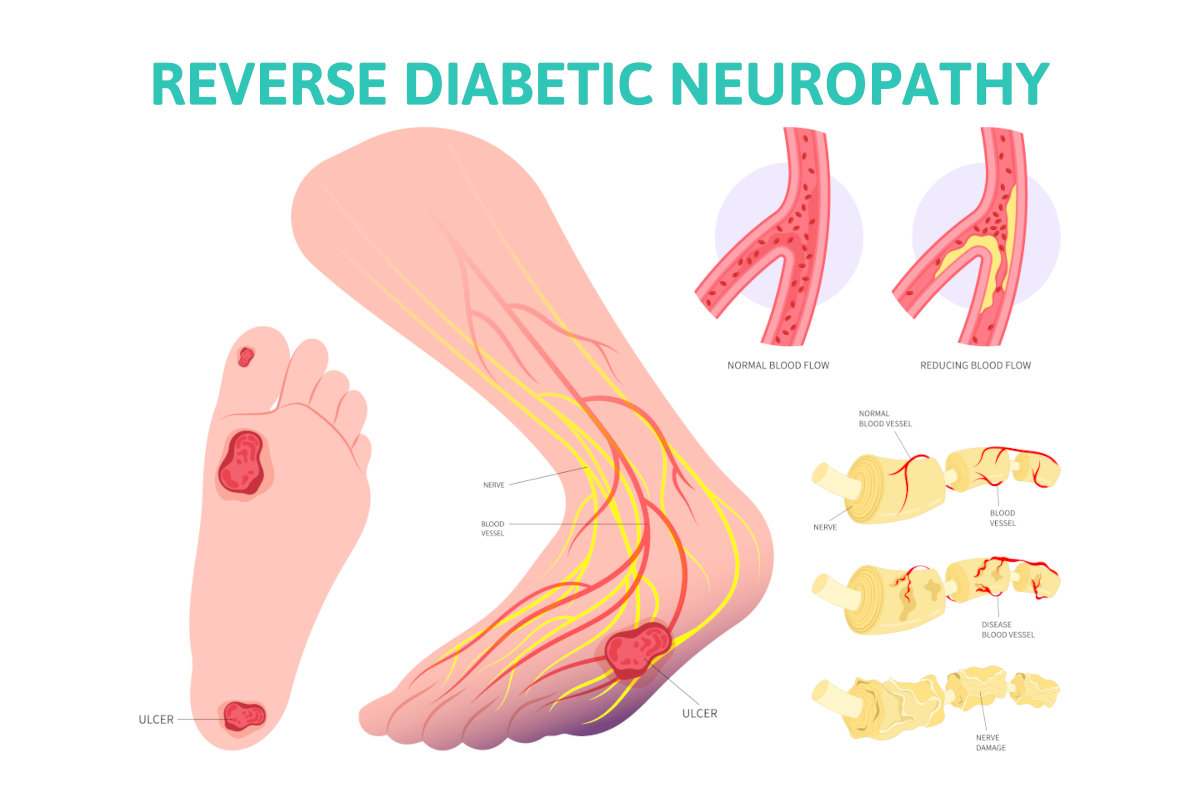
Diabetic neuropathy occurs when high blood sugar levels damage nerves throughout your body over the long term. The most common type is diabetic peripheral neuropathy, which primarily affects nerves in your feet and legs. This nerve damage can severely impact your ability to feel pain, temperature, and touch.
The condition affects nerves that control various body functions. When blood vessels that supply these nerves become damaged, it leads to the characteristic symptoms many patients experience. Managing your blood sugar levels is crucial, as elevated glucose damages both blood vessels and nerve fibers over time.
Types of Diabetic Neuropathy
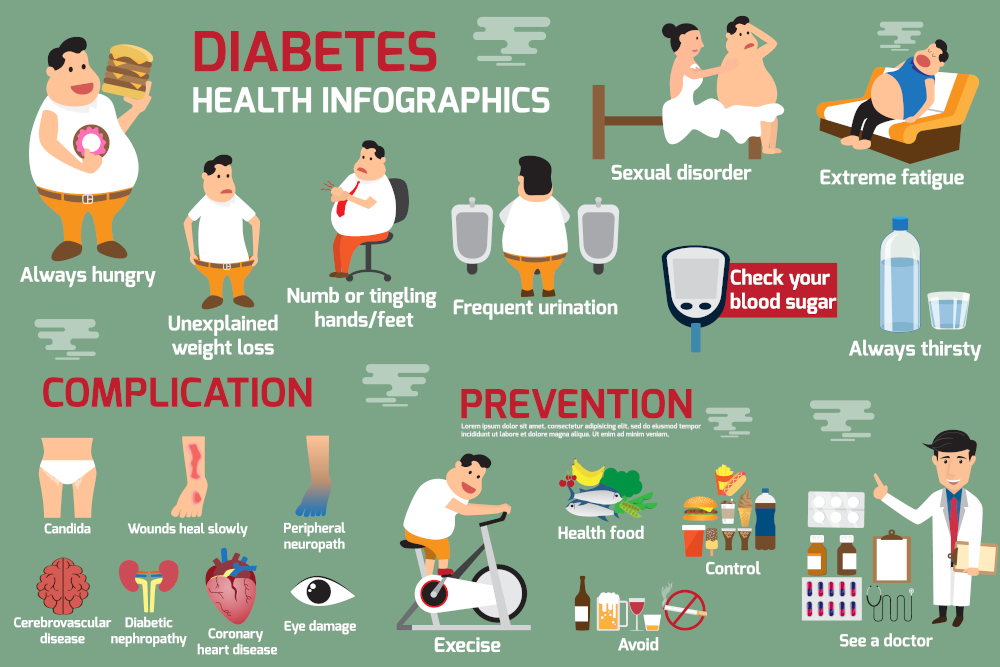
There are several types of diabetic neuropathy, and symptoms depend on the type affecting you:
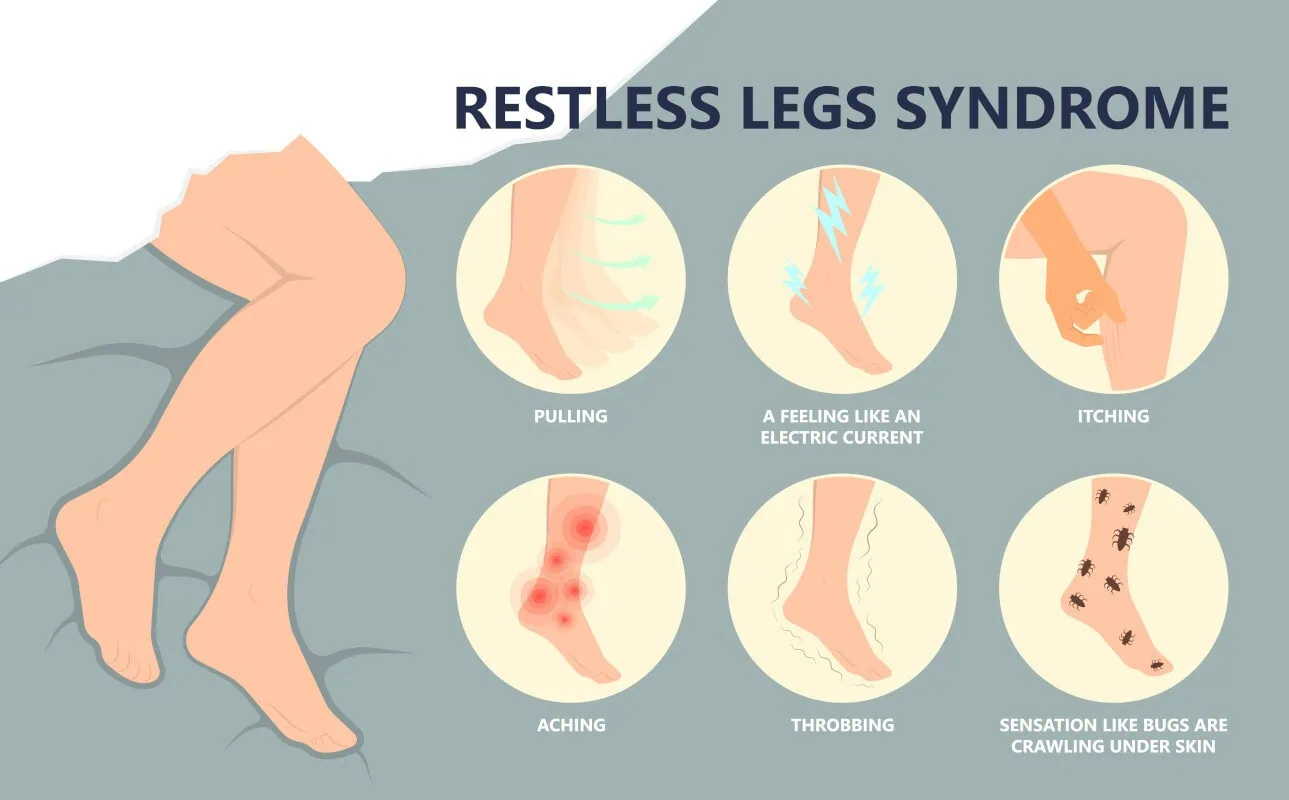
Peripheral Neuropathy: The most common type, causing numbness, burning sensations, and sharp pains in feet and legs. Many patients report symptoms become worse at night.
Autonomic Neuropathy: This type affects nerves that control internal organs, including blood pressure heart regulation, digestive system, and sex organs. It can impact bladder control and sexual function.
Proximal Neuropathy: Affects nerves in the hips, thighs, and buttocks, causing sudden weakness and pain.
Focal Neuropathy: Targets specific nerves, creating localized weakness or pain in particular areas.
Understanding which type affects you helps doctors create the most effective treatment plan for your specific situation.
Why Feet Are Most Vulnerable
Your feet bear the brunt of diabetic neuropathy for several reasons. The longest nerves in your body extend to your feet, making them most susceptible to damage from high blood sugar. Additionally, blood vessels supplying these distant nerves often sustain damage first, reducing oxygen and nutrient delivery to nerve tissues.
This nerve damage impairs your ability to feel pain properly, which normally serves as a protective warning system. Without this protection, minor injuries can go unnoticed and develop into serious complications.
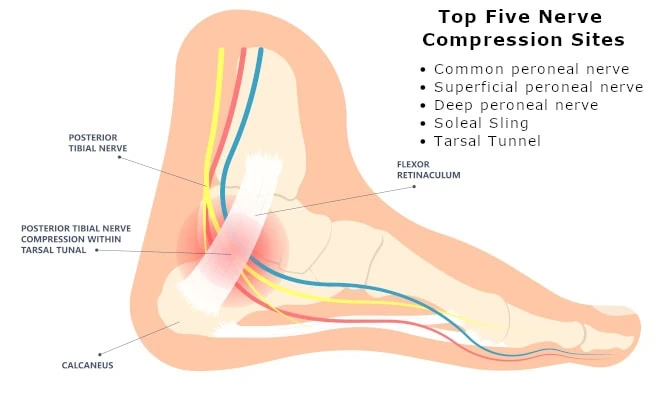
Breakthrough Research: Dr. James Anderson’s Nerve Decompression
Recent groundbreaking research by Dr. James Anderson, DPM, has revolutionized treatment approaches for diabetic nerve pain in feet. His work focuses on nerve entrapment, where damaged nerves become compressed in anatomical tunnels throughout the lower legs and feet.
Dr. Anderson’s research demonstrates that nerve decompression surgery can significantly improve symptoms by relieving pressure on compromised nerves. This surgical technique targets specific compression points, improving blood flow and reducing nerve irritation.
Benefits of Nerve Decompression Surgery
Patients who undergo Dr. Anderson’s nerve decompression procedures often experience:
- Restored sensation in feet and toes
- Significant reduction in burning and stabbing pains
- Lower risk of foot ulcers and potential amputations
- Improved balance and walking stability
- Potential restoration of some lost nerve function
Early intervention produces the best outcomes, emphasizing the importance of seeking treatment before irreversible damage occurs.
Essential Foot Care for People with Diabetic Nerve Pain In Feet
Proper foot care remains fundamental for anyone managing diabetic peripheral neuropathy. Daily inspection helps identify problems early, before they become serious complications.
Daily Foot Care Routine:
- Examine feet thoroughly for cuts, blisters, or color changes
- Keep feet clean and completely dry
- Wear properly fitted, supportive footwear
- Never walk barefoot, even indoors
- Moisturize feet but avoid areas between toes
These simple steps can prevent minor issues from becoming major complications that threaten your mobility and independence.
Comprehensive Treatment Approaches For Diabetic Nerve Pain In Your Feet
Managing diabetic nerve pain in feet requires a multi-faceted approach combining various treatment options:
Blood Sugar Management: Maintaining stable blood sugar levels remains the cornerstone of preventing further nerve damage. Work closely with your healthcare team to optimize your diabetes management plan.
Medication Options: Several medications can help manage neuropathy pain, including specific pain relievers, certain antidepressants, and anti-seizure medications that affect nerve pain signals.
Physical Therapy: Targeted exercises improve strength, balance, and mobility while helping maintain nerve function in affected areas.
Topical Treatments: Creams containing capsaicin or lidocaine patches can provide localized pain relief for some patients.
Nutritional Support: Certain vitamins and supplements may support nerve health, though you should discuss these options with your physician before starting any new supplements.
Managing Related Health Concerns
Diabetic neuropathy often affects more than just your feet. Autonomic neuropathy can impact blood pressure heart function, digestive processes, and sex organs. Working with your healthcare team to address these interconnected issues improves your overall quality of life.
Regular monitoring of blood pressure, heart health, and other organ functions helps detect and treat complications early. This comprehensive approach ensures you receive the most effective care for all aspects of your condition.
Hope for the Future
Thanks to pioneering research from specialists like Dr. James Anderson, treatment options for diabetic nerve pain in feet continue expanding. Nerve decompression surgery represents just one exciting advancement offering hope for symptom improvement and potential nerve function restoration.
The key to success lies in early intervention and comprehensive care. If you experience symptoms of diabetic neuropathy, don’t wait for them to worsen. Speak with your healthcare provider about all available treatment options, including advanced surgical techniques that might be appropriate for your situation.
With proper foot care, diligent blood sugar management, and access to cutting-edge treatments, living well with diabetic neuropathy is increasingly possible. Take control of your condition today by exploring all available options and working with specialists who understand the latest advances in neuropathy care. View more informational and testimonial videos on our YouTube Channel.
Watch Our Informational Videos On Nerve Pain From Diabetic Neuropathy
Schedule Your Appointment To Treat Diabetic Nerve Pain In Feet
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.

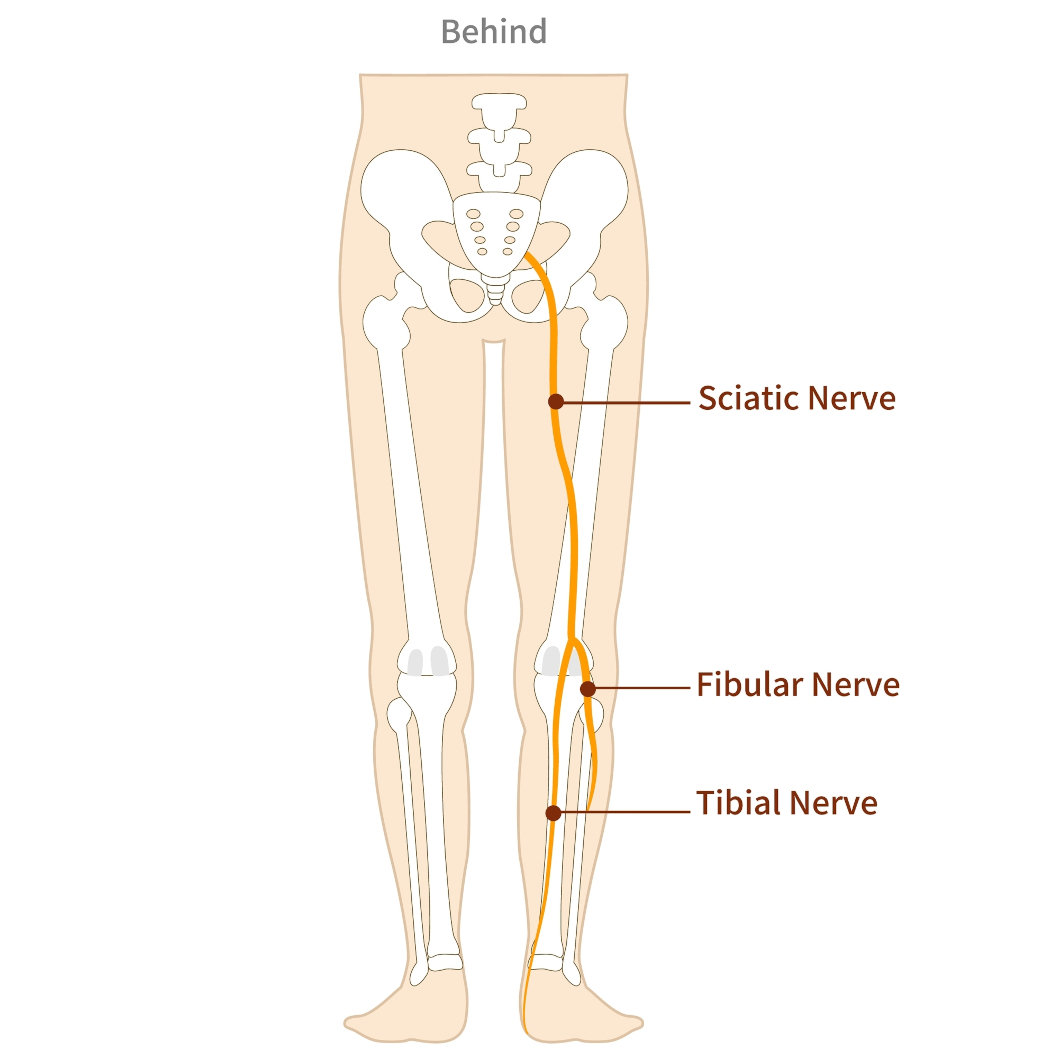


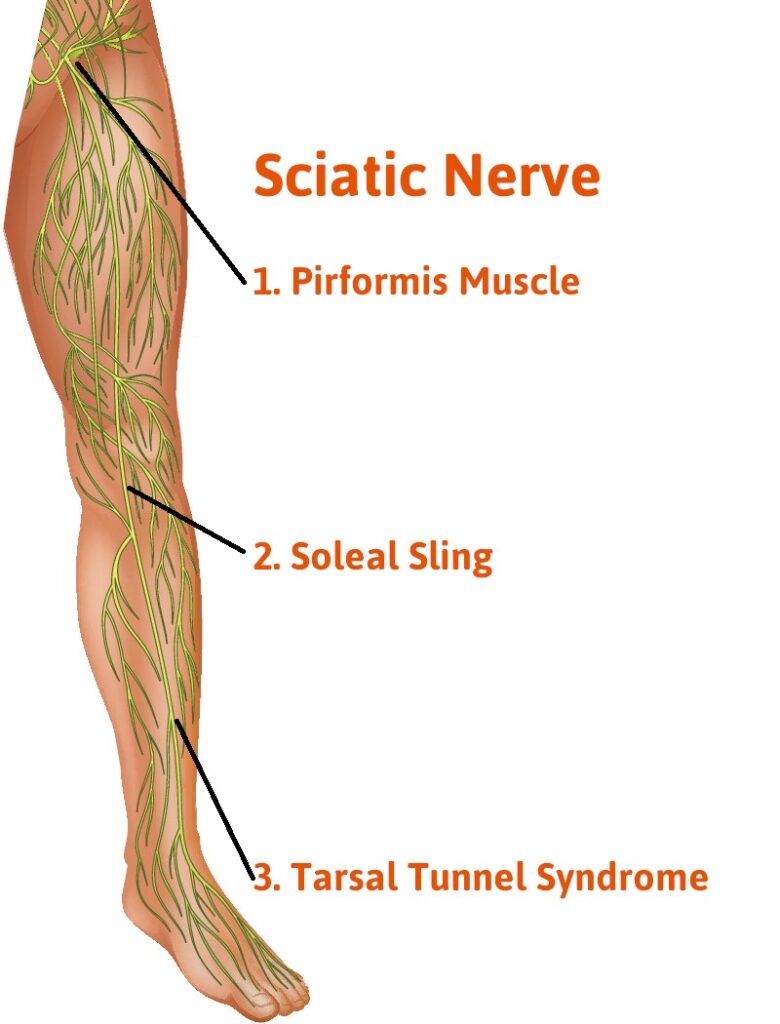

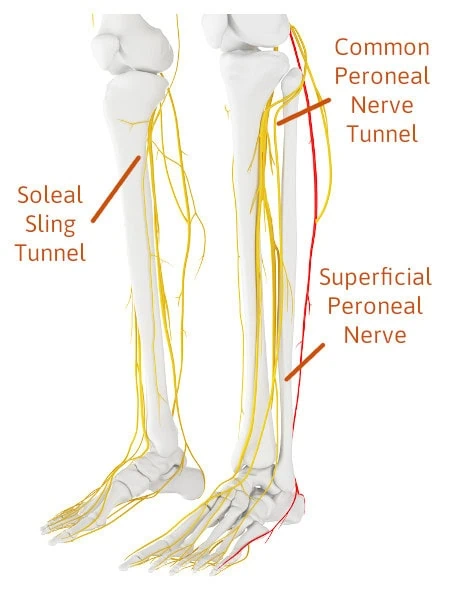 Three Nerve Tunnels In The Legs You Need To Become Familiar With To Understand The Source Of Your Leg Pain
Three Nerve Tunnels In The Legs You Need To Become Familiar With To Understand The Source Of Your Leg Pain