Your thinking about heel spur pain is all wrong!
Heels spur pain is one of the most common foot problems. It is a type of pain that often occurs when you first step out of bed in the morning. The pain can be excruciating and can find you limping to the bathroom. It can also happen later in the day. And oftentimes, if you have been active one day, say you went out for a run or a hike or a walk, and it was longer than normal, you can expect the same problem in the morning, but this time it’s worse. It can go on for months or years. But what is really happening inside your foot. This blog will open your eyes to some misconceptions about heel spur pain.
Why do I have a heel spur?
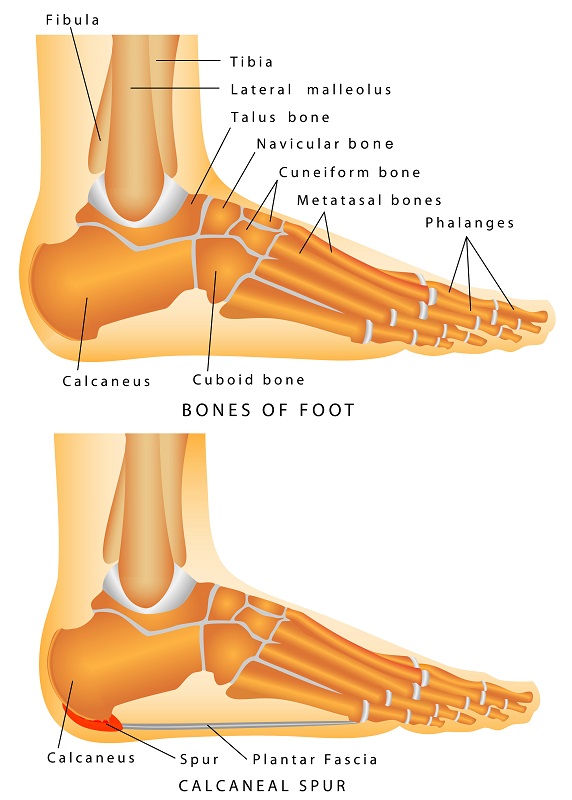 Let’s start with the basics. Many of you have heard of plantar fasciitis. The plantar fascia is a strong fibrous band of tissue that runs along the bottom of your foot starting in the ball and attaching to the bottom of the heel. With every step you take as the arch flattens the fascia is being pulled. When you are a teenager or child its very flexible like a rubber band but as you get older it loses its elasticity and starts to pull from where it attaches to the heel. So, let’s discuss the actual heel spur. Many patients will have a heel spur on the bottom of the heel on x-ray. This is a calcium deposit that may occur from the constant pulling of the fascia on the heel in this location. It is a bony protrusion that extends from the heel bone towards the toes. Another theory is that there can be microfractures in the heel from the fascia pulling so hard and the spur in a result of the heel bone attempting to repair. So, the most current understanding is that the actual spur is seldom if ever the true source of your pain. It is the result of the fascia pulling from the bone. What is the evidence to support this?
Let’s start with the basics. Many of you have heard of plantar fasciitis. The plantar fascia is a strong fibrous band of tissue that runs along the bottom of your foot starting in the ball and attaching to the bottom of the heel. With every step you take as the arch flattens the fascia is being pulled. When you are a teenager or child its very flexible like a rubber band but as you get older it loses its elasticity and starts to pull from where it attaches to the heel. So, let’s discuss the actual heel spur. Many patients will have a heel spur on the bottom of the heel on x-ray. This is a calcium deposit that may occur from the constant pulling of the fascia on the heel in this location. It is a bony protrusion that extends from the heel bone towards the toes. Another theory is that there can be microfractures in the heel from the fascia pulling so hard and the spur in a result of the heel bone attempting to repair. So, the most current understanding is that the actual spur is seldom if ever the true source of your pain. It is the result of the fascia pulling from the bone. What is the evidence to support this?
Three reasons to prove your heel spur does not hurt.
- Surgery – approximately ten percent of patients we treat have surgery when conservative measures fail. Surgery is performed endoscopically. The surgeon makes one or two small incisions and then releases a portion of the fascia. Patient may ambulate in a cam walker. This procedure allows the fascia to stretch and has an extremely high success rate. Many patients that have this done have a spur that is left. So, its not the spur.
WE’VE BEEN DOING THIS PROCEDURE FOR 30 YEARS.
- Regenerative medicine treatments – We now know that the fascia is not inflamed. Dr. Harvey Lemont (DPM)1 did a study that involved taking specimens of the fascia when he did surgery. Out of 50 specimens only one showed inflammation, fasciitis. Forty-nine of the specimens show degeneration of the fascia. We call this plantar fasciosis. Starting 10 years ago we changed our approach to treatment and have shifted away from the use of cortisone injections to use of regenerative medicine. Currently we use placenta cells as this helps to repair the tissues that are degenerating.
- Diagnostic ultrasound– Every patient we see has a evaluation of their heel ultrasound. This is the same technology used for mothers to see their child during pregnancy. The ultrasound will reveal the abnormal thickness and color that is associated with plantar fascia pain. This allows use the grade or rate the severity on the problem. Also the thickness of the fascia is reduced to more normal size after regenerative treatments.
Causes
The causes of heel pain can be multiple. If is often that that a tight calf and Achilles tendon can cause foot pain include heel spur pain. It may also be from improper foot biomechanics such as a foot that over pronates(flattens). Also, it can be from overuse or just the fact that as we get older its believed the fascia loses its elasticity. Also having tight calf muscles or Achilles tendon is thought to cause foot pain including heel pain.
Treatments
For some stretching or using a night splint you may get some relief. Also, some medical advice will be to use anti-inflammatories or do physical therapy. If you are currently doing any activity that involves running or jumping it may be suggested to take some time off these activities. Cortisone injections may also have some benefits. Using over the counter supports may also help.
We found these four treatments have had greatest success.
-
- Orthotics – Many podiatrists will recommend shoe inserts that we call orthotics. We are using a scanning technique that allows use to get a very precise measurement of your foot for these to be made.
- Regenerative medicine – We’ve been having success the use of stem in the form of placenta cell. We’ve been using regenerative medicine to repair the damaged fascia (plantar Fasciosis) for over ten years.
- Laser – Laser works by repairing the fascial tissue at a cellular level. Helping the energy producing part of the cell called the mitochondria the function better.
- Shockwave treatment – has also been phenomenally successful. Shockwave comes from the technology called lithotripsy which is used to break up kidney stones. Powerful sound waves are transmitted into the bottom of your heel and the trauma it creates stimulates your own body to want to repair the damaged tissue(fascia). It is believed that your own bodies growth factors and stem then are stimulated to repair the tissues. Finally, to use of laser can also be considered.
Surgery – Finally, if conservative options fail we’ve had great success with surgical treatment. The procedure done endoscopically so we’re able to visualize the fascia through small incisions. The fascia is released so that it can stretch, and patients are able to bear weight in a camwalker.
As you can see, at Anderson Podiatry Center, we offer both conventional and non-conventional, more progressive concepts when it comes to plantar fasciitis, which we like to call plantar fasciosis. We use evidence-based treatments that have been proven with the latest’s science regarding your heel spur pain. And as you can tell from this blog you need to rethink the idea that it is a spur. Because of the multitude of options we have we have a greater chance of avoiding surgery for our patients.
So, if you’re stumbling around, suffering with plantar fascia pain , or what you might be commonly calling now heel spur pain, please give us a call and we’ll consult you to see which direction we should go with your treatment.
1 Lemont, Harvey. “Https://Pubmed.Ncbi.Nlm.Nih.Gov/12756315/.” National Library of Medicine, June 2003, pubmed.ncbi.nlm.nih.gov/12756315.












 What exactly is an ingrown toenail?
What exactly is an ingrown toenail?





