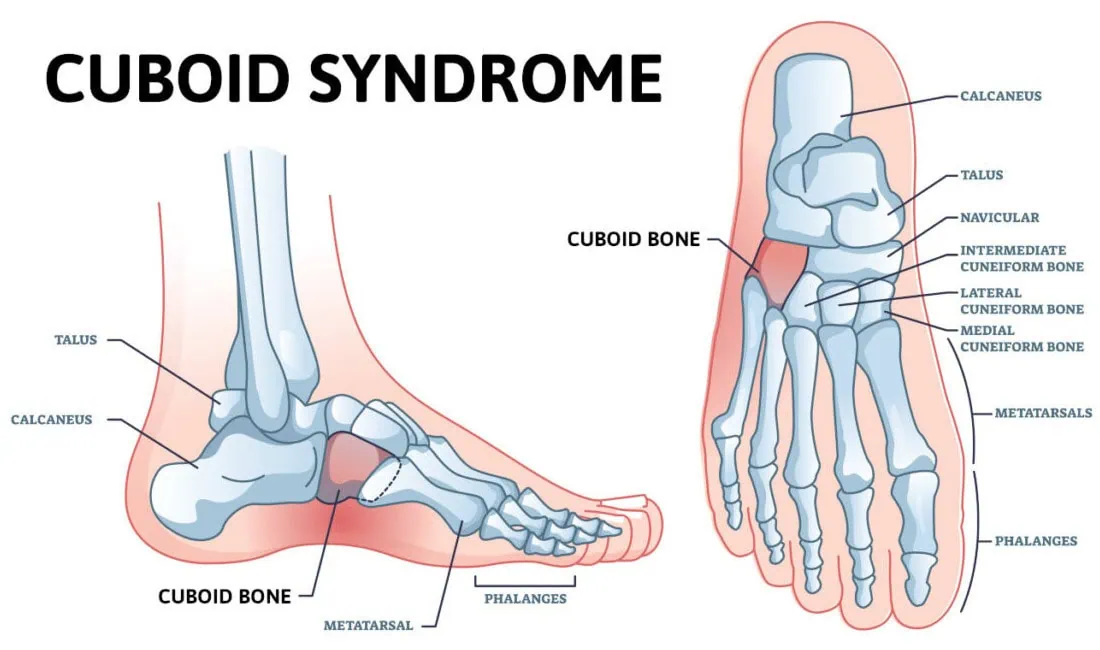
What is Cuboid Pain? Cuboid pain is not one of the most common foot complaints, but that’s why this blog is important for you to read. It’s a diagnosis that can be overlooked by healthcare professionals. The cuboid bone is a cube-shaped bone on the outside, lateral aspect of our foot – the pinky toe side of the foot. It lies halfway between our toes and heel. If you were to look at your foot from the side when you’re not bearing weight, it would be the bone that is at the highest part of your arch.
This area is called the lateral arch. The lateral arch is formed by the 4th and 5th metatarsal bones, which are the long bones that extend out to the ball of the foot that your bear weight is on. These two bones are connected to the cuboid bone by ligaments, and the bone forms the joint on the other side of the cuboid bone. The medial arch is the inner portion of the arch and is formed by the three metatarsal bones that connect to the midfoot. The medial arch is thought to be stronger than the lateral arch and can take more stress placed through this portion of the foot. This basic understanding is important to know as it plays a role in why you get cuboid pain. We will discuss the symptoms, diagnosis and cuboid syndrome treatment options in this blog.
What Happens When you Have Cuboid Syndrome Pain?
It is thought that the cuboid bone gets out of proper alignment with the calcaneus (heel) bone. This misalignment of the cuboid bone will cause pain in and around the joint. It can also be described as a midfoot sprain. It may also be referred to as cuboid subluxation.
Risk Factors for Cuboid Syndrome Include:
- Trauma– ankle sprains, often described as an inversion ankle sprain. When this occurs, the ankle twists in such a way that the body weight rolls towards the outer side of the foot on the small toes’ joint side. The added weight in this area can cause displacement of the calcaneocuboid joint. Other types of foot injuries may also be a cause.
- Foot biomechanics – individuals who overpronate or flatten their feet too much may be more prone to cuboid syndrome. It is thought that overpronation is the cause of cuboid pain for 80 percent of the population.
- Repetitive stress – overdoing it, especially with weight-bearing activities, can also lead to this problem. Ballet dancers are especially prone to this injury because of the positions the activity requires their feet to be placed in.
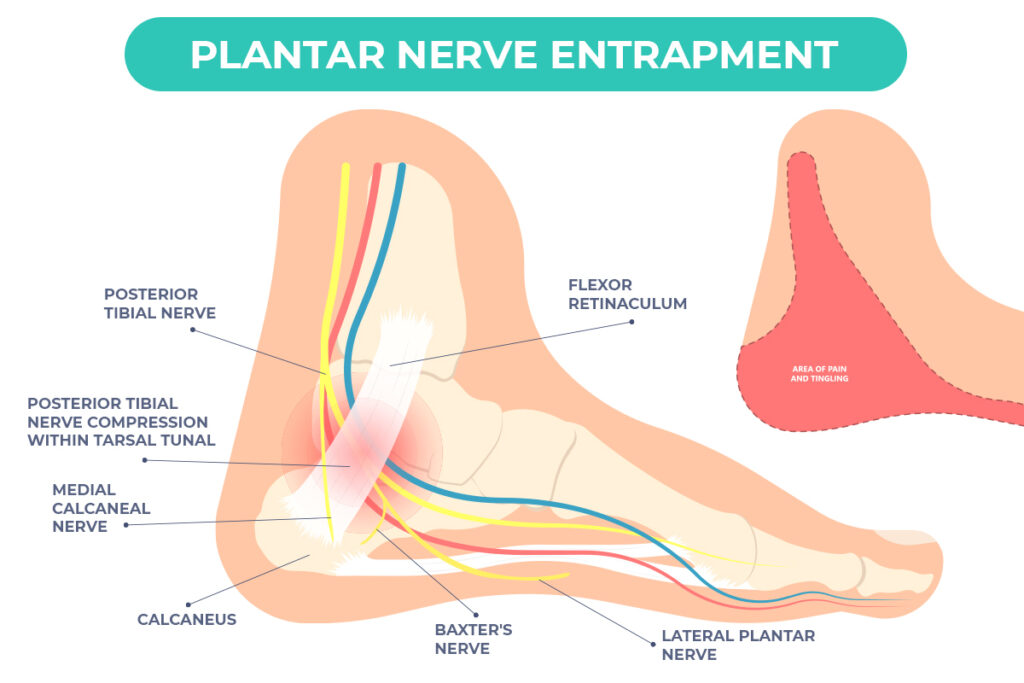
- Compensatory pain – one of the more common causes can be from pain elsewhere in the foot or ankle. We are very good at modifying our gait to help prevent pain. After a while, we may not even be aware we are doing it. If another foot problem requires us to walk on the outside of the foot to make it feel better, this may also be a cause. One example of this is plantar fasciitis. This will cause pain in the bottom of the heel, and it is common to compensate and avoid this pain by rolling your foot to the outside. If this is the case, it’s very important to resolve this pain first, and in many cases, this can fix the cuboid pain once the compensation stops.
What will my Symptoms be?
There will be pain on the outer side of the foot midway between the heel and the ball of the foot. The pain will occur when putting weight on the foot. It can be very severe and is usually a dull, deep pain. You may find you feel better when walking in shoes than barefoot as the support of the shoes may help with the discomfort.
How will the Doctor Diagnose Cuboid Syndrome?
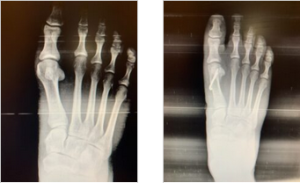
The doctor can learn a lot from your explanation of where the pain is. Also, examination of the foot will be important as the pain will tend to be directly over the calcaneocuboid joint. There may also be some swelling. X-rays will also be taken to rule out fractures of the cuboid or adjacent bones. Other problems that could mimic cuboid syndrome include a fracture of the cuboid bone, tendonitis of tendons in the area called peroneal tendons. MRI or diagnostic ultrasound may be used to evaluate these other problems to determine what cuboid syndrome treatment will be the most effective.
Mysterious Pain on the Outside of the Foot? Here are the Treatment Options for Cuboid Syndrome!
- Physical therapy – A physical therapist may be able to reduce pain in the cuboid area. This can also help to prevent the recurrence of cuboid syndrome.
This can be accomplished with
-
- Balance exercises – By improving balance, you will be less likely to injure your foot as ankle sprains can be a common cause of cuboid syndrome.
- Mobility exercises – To help regain full range of motion and get rid of any stiffness that may have occurred with cuboid syndrome.
- Strengthening exercises – this will provide more strength to support the foot and ankle. Stronger muscles and tendons will provide more support to the foot and ankle and reduce the chance of cuboid syndrome.
- Support of the cuboid bone – This may be accomplished by using padding underneath the cuboid bone area, over-the-counter arch supports may also help.
- Orthotics – Custom-made inserts to go in your shoes may be the most important part of the treatment that your podiatrist can provide. This can give very precise support to that portion of your foot and lead to full recovery. It must be emphasized that orthotics may be used to treat the primary problem that created the cuboid syndrome. A very common example would be if you’ve been favoring your heel (plantar fasciitis) and this compensation has put added stress on the cuboid area. Walking differently and favoring your heel makes it feel better, but now you have cuboid pain. So by eliminating the heel pain with orthotics, the cuboid pain goes away.
- Taping the foot and ankle – Taping the foot may also help support the calcaneocuboid joint area. This is especially effective in the early stage of the problem.
- RICE – Rest, ice, compression, and elevation may also be used. These treatments will reduce inflammation in the area and promote healing. For some, resting the foot for up to 6-8 weeks may be necessary before full recovery and returning to regular activities.
- Manipulation – This should only be attempted by a healthcare professional familiar with this technique. It is sometimes referred to as the cuboid whip. The technique involves placing the patient on their stomach with the knee on the involved side flexed. Then, with both hands gripping the foot, it is brought upwards and then thrust rapidly downward. This will allow the cuboid to pop back into its proper position.
- Modifying activities– Cross-training may also be helpful. If you’ve been doing weight-bearing activities that involve a lot of side-to-side motion which may stress the cuboid joint area more, you may elect to take a break and bike,
As with many foot and ankle injuries, cuboid syndrome should be properly diagnosed and treated as soon as possible. This will help to speed up getting back to full activities. So, if you’re having a mysterious pain on the outside of your foot please consider the possibility of cuboid syndrome. We have skilled podiatrist who guide each of our patients to ensure a proper cuboid syndrome treatment is chosen that best suits the individual.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.