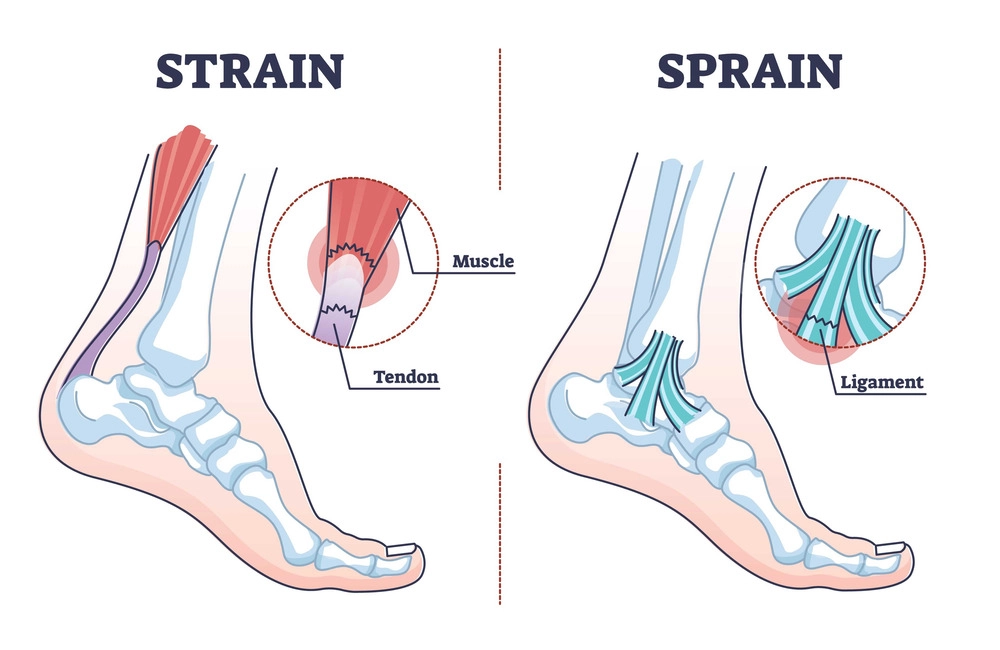
Foot ligament injury is a common problem in the foot and ankle. A ligament is a strong fibrous tissue whose function is to stabilize joints. A ligament is the tissue that connects the bones that form the joints. Ligaments can be injured from overuse but are more commonly injured from trauma. Ligament injuries are referred to as foot and ankle sprains. And out of all the possible ligament injuries, ankle sprains are the most common.
How Do I Know If I Have A Foot Ligament Injury In My Foot?
- You may feel or hear something pop or snap
- You may have pain and swelling in the area of injury
- Don’t assume if you can walk on your foot or ankle that the ligament is not injured
- It hurts when you put weight on your foot.
How Do We Know If The Ligament Is Injured?
It starts by taking x-rays in most cases to rule out bone injuries. X-rays may also be used to see if a joint has more motion in it than normal. These are called stress views and your local podiatrist will advise you after reviewing the results. This can indicate that the ligament is no longer stabilizing the joint, and this is sometimes done to evaluate ankle sprains. An MRI may be ordered. This can help the doctor know if it is a ligament that is injured, and the severity. There are three different grades of tearing depending on the severity of the injury. Grade 1 is the mildest and means most of the ligament is not torn. Grade 2 indicates that 40-60 percent of the ligament is torn. A large tear is grade 3 and this indicates that the tear is completely through the ligament.
Treatment Of A Foot Ligament Injury
The options for treatment of a foot ligament injury vary depending on the severity. The most severe tears may need immobilization for weeks using a Cam walker. Some doctors may even suggest surgical repair to reconnect the torn ligament ends to allow them to better heal. With a more minor tear such as a grade 1, resting, icing, and elevation with gradual return to physical activities may be all that is needed.
Ankle Sprains
Of all the potential ligament injuries of the foot and ankle, injuries to the ligaments of the ankle are most common. It’s important to consider if it’s the first ankle sprain you’ve had, or if you have a history of repeated sprains. If it’s your first one and it’s associated with severe pain and swelling, a sense of something popping or giving out is important to note. In this situation, you should be evaluated by a foot and ankle specialist. With a severe sprain, a complete tear would mean that immobilization in a Cam Walker may be recommended. This will allow the ligament ends to be in closer approximation and provide a better chance of full repair. Without proper treatment, you may now be left with an ankle joint that is chronically unstable. Without proper treatment from the beginning, the instability of the ankle may become chronic. In some cases, this might require surgery to stabilize the ankle. Ankle sprains tend to be the most under evaluated and undertreated foot and ankle injury. Patients often go to an emergency room or urgent care facility. If x-rays rule out a fracture, little after care may be given.
What You Can Do To Prevent Ankle Sprains?
- Consider wearing high top athletic shoes if you’re playing basketball
- Use an over-the-counter ankle brace
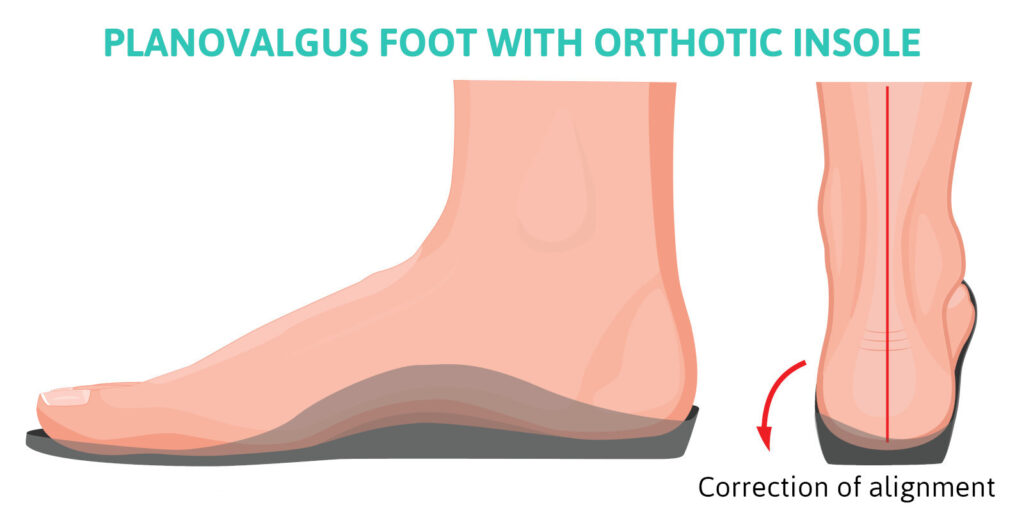
- Consider custom made orthotics as these give your feet better feedback regarding foot placement
- Do ankle exercises and consider trail hiking or running to build up muscle strength. This may help support your ankle joint more
So, it is important to understand that no matter where the foot ligament injury (ankle or foot) is, a ligament tear is to be suspected. Just because you can walk on it, and just because it’s not fractured doesn’t mean aggressive treatment wouldn’t be a good idea. As it’s often been said, a sprain can be almost as bad as a fracture. Finally, it is always better to error on the side of caution and consult with you podiatrist if you have concerns about a possible ligament injury.
Dr. Anderson, the founder of Anderson Podiatry Clinic, DPM, ABPS, FACFS, FAENS