Teamwork, Savings, And Great service – Why It All Really Matters!
When you’re needing surgery for your foot problems, having a surgical center within the clinic gives you an advantage. When non-surgical options such as physical therapy fail to give relief of your foot or ankle problems, surgery may become part of your treatment plan. Our surgeons are board certified foot and ankle surgeons who specialize specifically in the foot and ankle. We provide surgery for a variety of foot and ankle problems. Oh, and did I mention that all of our podiatric surgeries are day surgeries and require no overnight stay? That is what I mean by “the advantage”.
Not only do we have the top foot and ankle specialists, but our surgery center is also the only foot and ankle surgery center in Colorado. In fact, the only one in the entire rocky mountain region.
The Advantage
The Team Approach: As a patient, you may not be aware of the challenges a surgeon faces when needing to travel to various facilities in order to conduct their procedures. Each and every time they go, they will be faced with having staff who have no familiarity with them, and vice versa. Not to mention the staff may not specialize in the specific surgery that they may be conducting.
At Anderson Podiatry Center, our staff is here for us when it comes to day-to-day patient care, and for surgery. They have been selected and trained by us for our specialized needs during surgery. This team approach helps us to serve our patients better in the operating room. They are knowledgeable on every surgical procedure we do!
 Savings Cost transparency this is the new “buzzword” in healthcare, but nothing new at Anderson Podiatry Center. We have been offering bundled pricing for many years.
Savings Cost transparency this is the new “buzzword” in healthcare, but nothing new at Anderson Podiatry Center. We have been offering bundled pricing for many years.
What is bundled pricing?
Simply stated, we include the surgeons’ fees, anesthesia fees, and facility fees all together with one cost. There are no surprises. We have found our patients to be excited about this, as it seems to be the opposite approach when they get their services from big healthcare facilities. Also, in today’s world of high deductibles, patients may save money by not using their insurance in certain situations by instead simply paying out of pocket. Again, a significant cost savings.
We also offer services that are unique! Amongst the most popular include the reversal of restless legs, and neuropathy.
Many people travel here from throughout the United States and Canada without insurance, or because we are not part of their insurance plan. We always offer affordable pricing for many.
How can we offer such affordable pricing?
Let me explain: When you look at healthcare dollars in the past, 70% of those dollars went to the doctors and nurses who delivered the care, and 30% to the administration. Now the percentages have flipped. 70% goes to administration, and 30% to the doctors and nurses. At larger facilities you are paying for that administrative cost. In a smaller facility such as ours, we don’t have that administrative cost. That is how the cost saving can be passed on to you!
Great Service.
As a final thought, I think you’ll find our staff to be exceptional in their expertise and friendliness. We have the best staff around! Please consider our clinic and surgical center as your one-stop clinic for all your foot and ankle care.

 To begin, every patient we see with heel pain has an ultrasound examination of their heel. We know what the normal appearance of fascia should be by immense studies that have been performed. Generally, a patient with plantar fascia pain will have a thicker and darker appearing fascia in the area where it attaches to the heel bone. A diagnostic ultrasound is extremely useful to ensure that your pain is truly from fascia. If the fascia looks normal, we will then suspect the nerve problem.
To begin, every patient we see with heel pain has an ultrasound examination of their heel. We know what the normal appearance of fascia should be by immense studies that have been performed. Generally, a patient with plantar fascia pain will have a thicker and darker appearing fascia in the area where it attaches to the heel bone. A diagnostic ultrasound is extremely useful to ensure that your pain is truly from fascia. If the fascia looks normal, we will then suspect the nerve problem.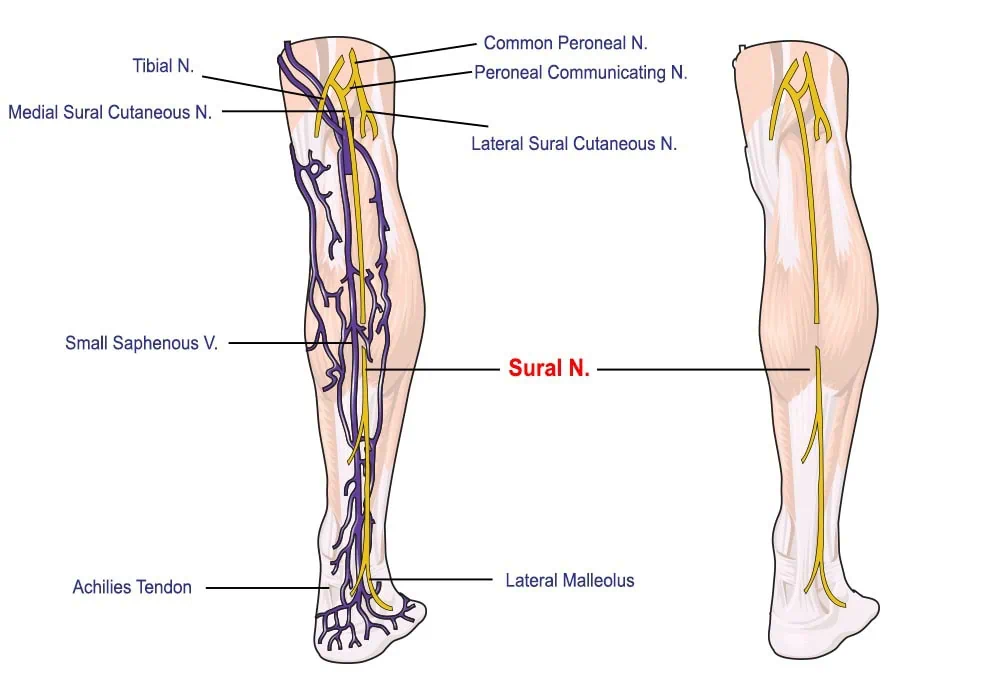

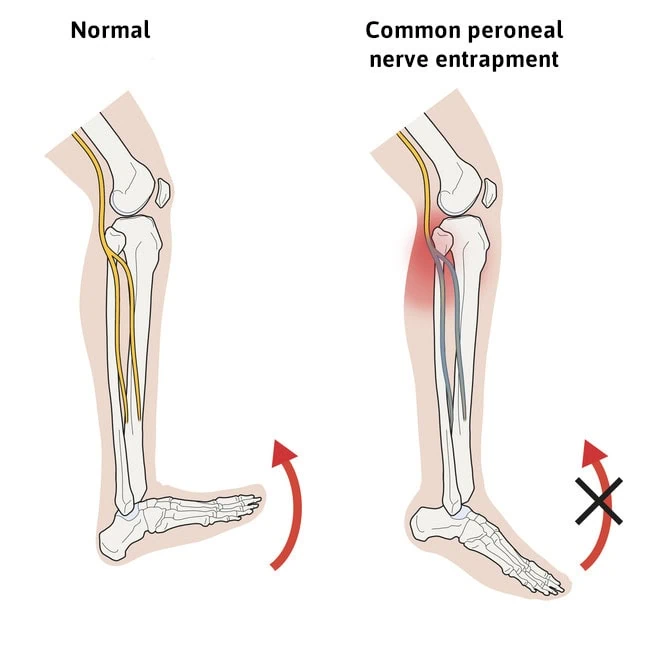

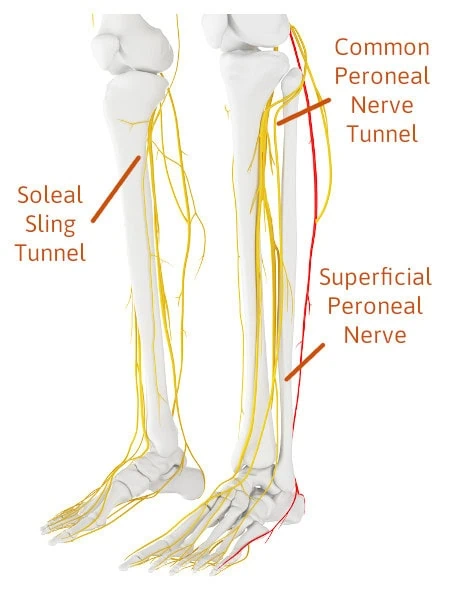 Three Nerve Tunnels In The Legs You Need To Become Familiar With To Understand The Source Of Your Leg Pain
Three Nerve Tunnels In The Legs You Need To Become Familiar With To Understand The Source Of Your Leg Pain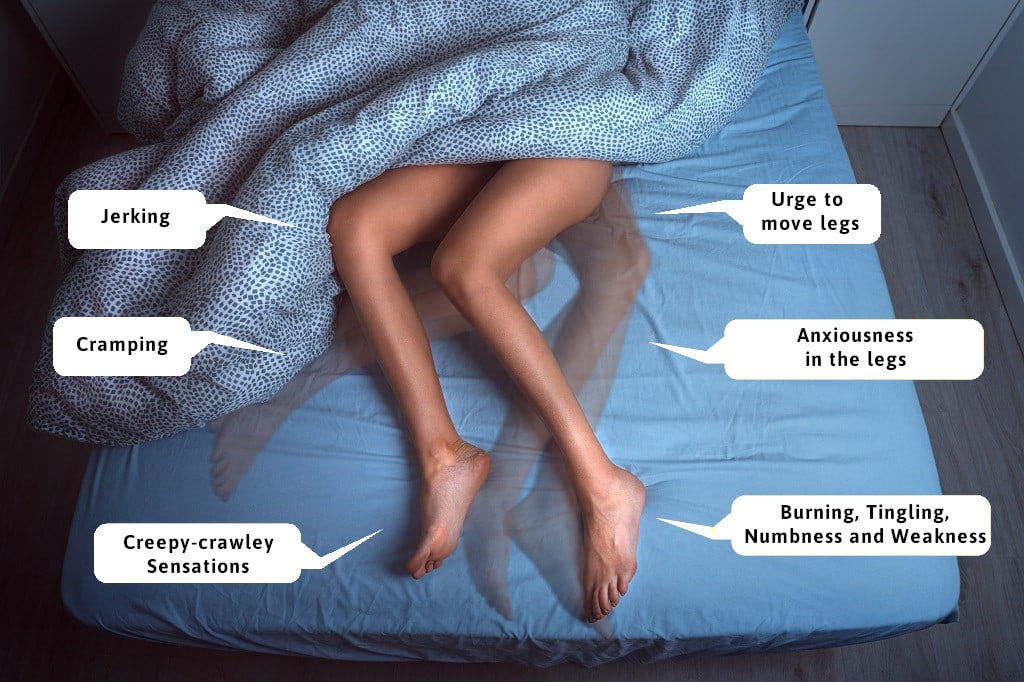
 Symptoms of Restless legs tend to present at night, and therefore, many suffer from lack of sleep. This can lead to exhaustion, depression, and other issues such as weight gain and high blood pressure. Most common symptoms include the urge to move the leg, which in turn means waking up. Additional symptoms could be “creepy crawly” sensations, cramping, and uncontrollable jerking (often referred to as periodic limb movement disorders). These symptoms either interrupt sleep, or make it difficult to fall asleep leading many to develop sleeping disorders.
Symptoms of Restless legs tend to present at night, and therefore, many suffer from lack of sleep. This can lead to exhaustion, depression, and other issues such as weight gain and high blood pressure. Most common symptoms include the urge to move the leg, which in turn means waking up. Additional symptoms could be “creepy crawly” sensations, cramping, and uncontrollable jerking (often referred to as periodic limb movement disorders). These symptoms either interrupt sleep, or make it difficult to fall asleep leading many to develop sleeping disorders.
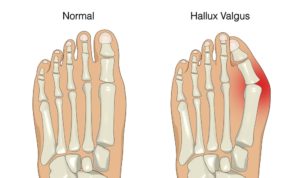 It is a popular notion that shoe gear is the primary reason one develops a bunion. However, most foot specialists agree that improper foot mechanics from inherited foot type plays a larger role. In fact, it has been noted in some cultures such as tribes in Africa and New Guinea, that shoes are rarely worn, yet bunions are still present within the populations. You may hear, “My mom had bunions and now I do too!”, as a pretty common phrase that goes around.
It is a popular notion that shoe gear is the primary reason one develops a bunion. However, most foot specialists agree that improper foot mechanics from inherited foot type plays a larger role. In fact, it has been noted in some cultures such as tribes in Africa and New Guinea, that shoes are rarely worn, yet bunions are still present within the populations. You may hear, “My mom had bunions and now I do too!”, as a pretty common phrase that goes around.