Put your best foot forward after reconstructive foot and ankle surgery

The purpose of reconstructive foot and ankle surgery is to restore normal function to the foot and ankle. It may also be needed to eliminate a painful condition and in some situations improve the cosmetics of the foot or ankle. Reconstructive foot and ankle surgery can be for soft tissues problems, structure problems and some conditions may be treated with minimally invasive techniques.
Soft tissue problems
 Soft tissue foot reconstructive surgeries may include treatment for ganglions and fibromas. Ganglions can originate from a tendon sheath or from joint capsule. In some cases, the doctor may be able to aspirate the fluid out with a needle in an office setting but if the problem returns or the ganglion is large surgical excision may be the treatment of choice. This can help with the pain and cosmetically improve the look of the foot or ankle.
Soft tissue foot reconstructive surgeries may include treatment for ganglions and fibromas. Ganglions can originate from a tendon sheath or from joint capsule. In some cases, the doctor may be able to aspirate the fluid out with a needle in an office setting but if the problem returns or the ganglion is large surgical excision may be the treatment of choice. This can help with the pain and cosmetically improve the look of the foot or ankle.
A fibroma may occur on the bottom of the foot is known as Ledderhose disease or plantar fibromatosis. Seldom is surgery to remove the mass necessary but in most cases the use of an injection with a specific enzyme to dissolve the growth can be very successful.
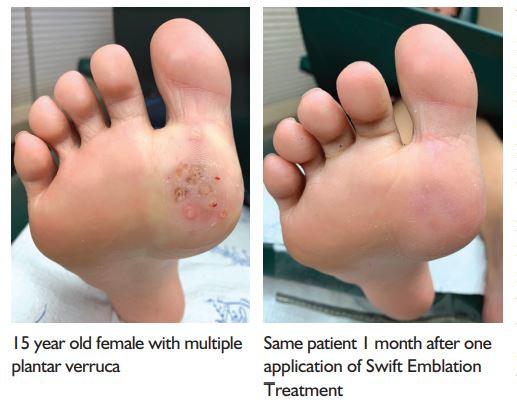
Warts can also be very unsightly and painful. In the past treatment options have included, excision, use of chemicals that destroy the wart or freezing. These are all destructive in nature, however, with the advancement of technology the use of microwave energy with the SWIFT® device is used. It is the preferred option because it helps the body’s immune system have a more aggressive response to the wart virus. The patients’ own immune system eliminates the wart! Treatment with the SWIFT® device is in the office and allows the patient to walk immediately with no down time.
Structural problems

The most common foot reconstructive surgeries may include bunions and hammertoes. Bunions usually require the use of pins, bone screws or plates to correct the alignment of the boney structure. View our patient testimonial from Kari on bunion surgery completed for both feet!
Hammertoe procedures may need a minimally invasive technique requiring a small incision to release a tendon that has become too tight or removal of a boney segment from the toe or fusion of one of the digital joints may be needed in more severe cases.
Hallux rigidus is also a painful foot complaint that results in a great toe joint that is stiffer and arthritic. Surgery may be needed to remove the unsightly boney growth from the top of the great toe joint and reposition the joint with the use of pins or bone screws. The result is pain-free motion and elimination of the bump. Flatfoot surgery may also be needed for a flatfoot that has been acquired as a birth defect or has progressed over a lifetime. Flatfoot reconstructive surgery may be as simple as using an implant in a joint beneath the ankle joint to block flattening of the arch or may involve procedures that require tendon lengthening’s with the use of bone grafts and even bone fusions in some situations. These procedures may require more recovery time.
Minimally invasive procedures
A very common complaint is heel pain. This is referred to as plantar fasciitis. When conservative measures fail two small incisions on either side of the heel are made and a scope is then inserted into the foot so that the fascial tissue can be released. This allows the fascia to be lengthened reducing its excessive pulling from the heel bone. Small incisions may also be used to help with ankle surgery. A scope is placed into the joint and the surgeon then then repair the damage if the joint is arthritic or has inflammatory tissue. Both procedures may require minimal recovery time with the patient ambulating soon after surgery.
Joint denervation surgery – Avoiding ankle replacement surgery!
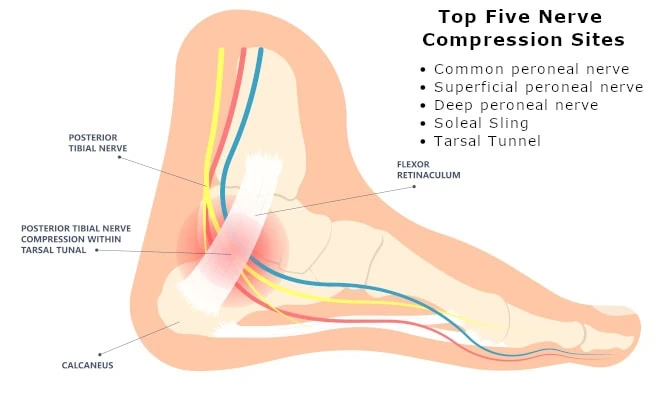
This involves the blocking of pain signals to the brain by the resection of one or more nerve branches through small incisions just above the ankle joint. The nerves have no motor function therefore there is no resulting weakness after the procedure. Many of our patients are choosing this before considering procedures such as ankle replacement surgeries.
Yes, surgery may require significant recovery time. However, the good news is that with technology and surgical innovation you may have less recovery time needed than in the past. If you would like help considering all the options that are now available, please allow us to guide you through the decision process. You may be surprised that your condition can be addressed with minimally invasive technique or by non-surgical means.