 Twitches are common. Muscle twitching is a common complaint that can be associated with restless legs (RLS). You do not have to have restless legs to have muscle twitching, but it can be a symptom related to restless legs that is annoying, and in its more severe forms can present as jerking in the legs. Another term to describe this is periodic limb movement disorder (PLMD). Another common medical term to describe muscle twitching is muscle fasciculations. Both muscle twitching and muscle fasciculations can be used interchangeably. Muscle twitching can be in different parts of the body. In this blog, we will specifically focus on muscle twitching and how it relates to restless legs syndrome but before we do so we need to mention other medical conditions or reasons that you may be getting muscle twitching in your leg.
Twitches are common. Muscle twitching is a common complaint that can be associated with restless legs (RLS). You do not have to have restless legs to have muscle twitching, but it can be a symptom related to restless legs that is annoying, and in its more severe forms can present as jerking in the legs. Another term to describe this is periodic limb movement disorder (PLMD). Another common medical term to describe muscle twitching is muscle fasciculations. Both muscle twitching and muscle fasciculations can be used interchangeably. Muscle twitching can be in different parts of the body. In this blog, we will specifically focus on muscle twitching and how it relates to restless legs syndrome but before we do so we need to mention other medical conditions or reasons that you may be getting muscle twitching in your leg.
- Amyotrophic Lateral Sclerosis (ALS), or also known as Lou Gehrig’s Disease – This is a severe neurological condition that includes speech difficulties such as slurred speech and difficulty speaking. It can also cause muscle weakness that can become severe in the hands, arms, feet, and legs. If you are having significant weakness of muscles or difficulty speaking, this could lead you to suspect ALS.
- Increased adrenaline – Anything that stimulates the body such as caffeine or stress may also be a cause of muscle twitching.
- Fatigue – Any type of activity that may cause muscle fatigue may result in muscle twitching along with muscle spasms and muscle cramps after the activity is completed.
- Benign Fasciculation Syndrome – This is a medical condition that can cause fasciculations in various muscle groups of which there is no known cause.
Treatment of muscle twitching in legs
Because these symptoms are not serious, there aren’t any FDA-approved treatments that are known to stop muscle twitching. There may be medications that are used to relax the muscles and reduce muscle twitching. However, the side effects of these medications are not worth the benefits.
Muscle Twitching/Jerking as it relates to Restless Legs
A New Hypothesis
To understand muscle twitching as it relates to restless legs, we first must understand the two basic anatomical components of the nervous system.
Central Nervous System
The central nervous system is composed of the brain and the spinal cord. Most research regarding restless legs involves the central nervous system. It is thought that lower dopamine levels or lower iron levels in the brain may correlate to having restless legs. Oftentimes medications are used to increase dopamine levels or iron levels in the brain.
Peripheral nervous system
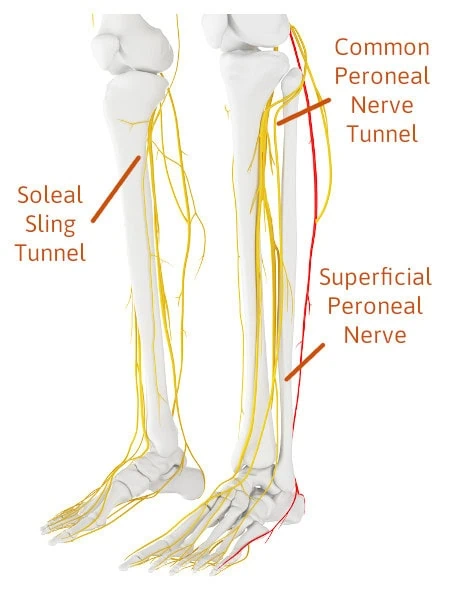
The peripheral nervous system is composed of nerves that extend to the arms and legs. An example in the upper extremity is the median nerve in the wrist which undergoes compression as it passes through a tunnel called the carpal tunnel. Another area is the ulnar nerve in the elbow which is also referred to as the funny bone when you hit your elbow. This new idea about jerking or twitching is that it may be caused by damage to the nerves of the peripheral nervous system.
Background
This author has successively reversed the symptoms of neuropathy for over two decades. The symptoms of neuropathy are reversed by opening (decompressing) different nerve tunnels in the lower extremity. By releasing the compression on these nerves, the symptoms of neuropathy can be improved. Approximately ten years ago, it was found that two additional nerve tunnels could be causing nerve compression and seem to be highly correlated to restless legs. By relieving pressure on the nerves in these two tunnels, reversal of restless legs symptoms was possible. Not only were the symptoms of nervousness, restlessness, creepy crawly sensations, and cramping released but also jerking and fasciculations were also reduced or eliminated.
How This Concept Disrupts Conventional Medicines Theory on Twitching and Jerking related to Restless legs?
Until the recent observation of patients having great success with nerve decompression surgery helping restless legs, it had always been assumed that iron and dopamine may play a major role. That is not to say that they may have some impact, however, it is important to note that surgical decompression has shown success and should be considered an option especially when restless legs symptoms are severe.
The new hypothesis for muscle twitching in the leg.
The idea is that the twitching can be caused by the peripheral nervous system when the nerves are damaged from excessive compression. This damage to the nerve may cause a noxious sensation in the legs and send a signal to the spinal cord and the central nervous system that results in a twitching or jerking response in the muscles in the leg.
In some cases, severe jerking is involuntary meaning it cannot be controlled by the patient. Another possibility is that the compression also damages the motor neurons that stimulate muscle contraction. This may also create twitching and lead to muscle weakness which is seen in some patients with restless legs. With the noxious stimuli, if it is mild, the patient may present with fasciculations. Currently, we have one peer-reviewed published paper showing the fact that we can reverse restless legs symptoms, and another paper soon to be published. Both papers report that jerking is eliminated or greatly reduced.
So, if you have severe symptoms of restless legs that are affecting your sleep and also there is twitching in your legs, understand that there may be another option. This new option of decompression of tight nerve tunnels in the legs tells us there’s a possibility that the twitching may be related to the compression of the nerve. I often refer to restless legs as restless legs compression syndrome as for many there is compression in the nerve tunnels in the legs where the symptoms of restless legs are found.
Experiencing unexplained muscle twitching in your legs? Our foot and nerve specialists can help pinpoint the cause and find a solution.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.
David Post Operation
Arlene is cured of muscle twitching in her legs after 25 years


 Three Nerve Tunnels In The Legs You Need To Become Familiar With To Understand The Source Of Your Leg Pain
Three Nerve Tunnels In The Legs You Need To Become Familiar With To Understand The Source Of Your Leg Pain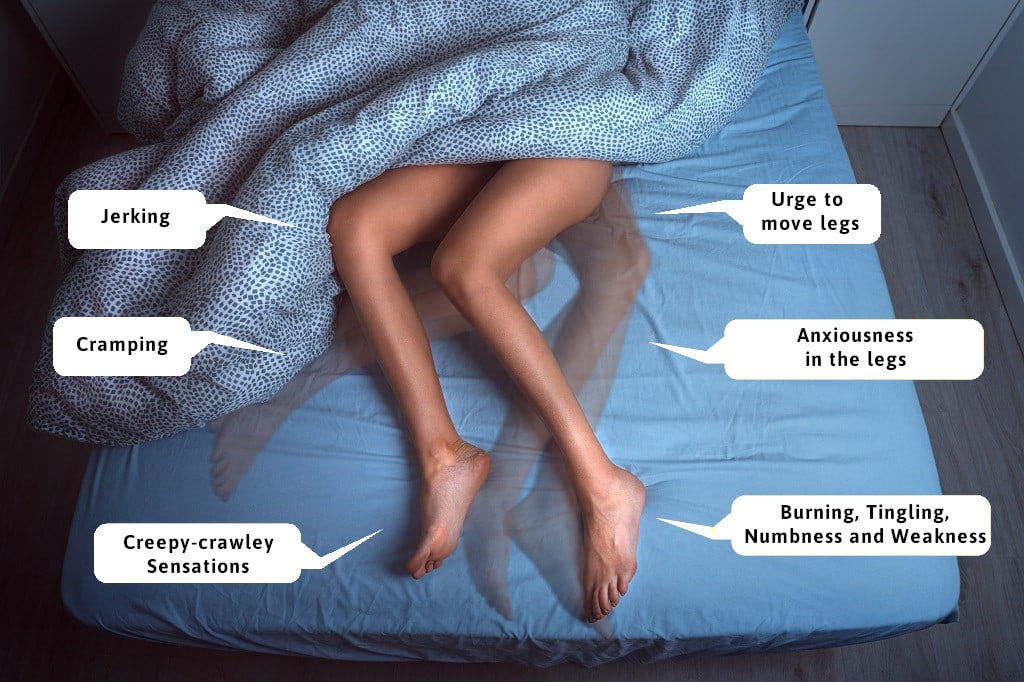
 Symptoms of Restless legs tend to present at night, and therefore, many suffer from lack of sleep. This can lead to exhaustion, depression, and other issues such as weight gain and high blood pressure. Most common symptoms include the urge to move the leg, which in turn means waking up. Additional symptoms could be “creepy crawly” sensations, cramping, and uncontrollable jerking (often referred to as periodic limb movement disorders). These symptoms either interrupt sleep, or make it difficult to fall asleep leading many to develop sleeping disorders.
Symptoms of Restless legs tend to present at night, and therefore, many suffer from lack of sleep. This can lead to exhaustion, depression, and other issues such as weight gain and high blood pressure. Most common symptoms include the urge to move the leg, which in turn means waking up. Additional symptoms could be “creepy crawly” sensations, cramping, and uncontrollable jerking (often referred to as periodic limb movement disorders). These symptoms either interrupt sleep, or make it difficult to fall asleep leading many to develop sleeping disorders.


