Treating the root of the problem for an achilles tendon injury
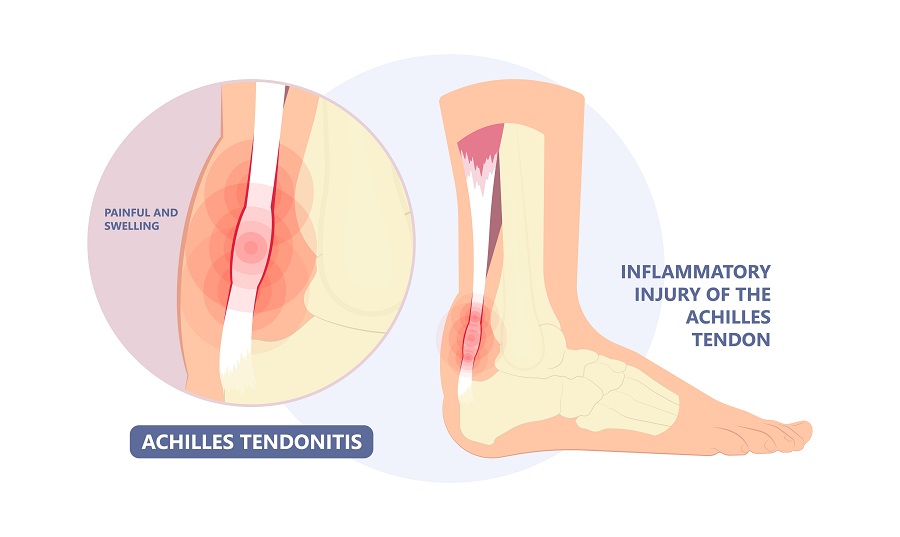 The Achilles tendon originates from the large calf muscles in the back of the lower leg and attaches to the back of the heel bone. Its function is to push your heel up off the ground and to propel you forward. Pain can occur along the tendon, that band of tissue just below the calf muscle, or where the tendon attaches to the heel bone. The pain can be very disabling, not allowing you to walk or run anymore and or do other activities. It may limit the range of motion in your ankle because of the pain. You may also notice swelling of the tendon associated with your pain. If the back of the heel bone appears enlarged, it may be from the Achilles tendon. So even though a heel spur or boney growth on the back of the heel may be noted it is now thought that in many cases the pain is from the tendon. These problems are referred to as a Haglund’s deformity or a retrocalcaneal spur. This goes against much of conventional medicine as our approach but the high success rate of our treatments for an achilles tendon injury that are directed at treating the tendon and not the bone prove otherwise.
The Achilles tendon originates from the large calf muscles in the back of the lower leg and attaches to the back of the heel bone. Its function is to push your heel up off the ground and to propel you forward. Pain can occur along the tendon, that band of tissue just below the calf muscle, or where the tendon attaches to the heel bone. The pain can be very disabling, not allowing you to walk or run anymore and or do other activities. It may limit the range of motion in your ankle because of the pain. You may also notice swelling of the tendon associated with your pain. If the back of the heel bone appears enlarged, it may be from the Achilles tendon. So even though a heel spur or boney growth on the back of the heel may be noted it is now thought that in many cases the pain is from the tendon. These problems are referred to as a Haglund’s deformity or a retrocalcaneal spur. This goes against much of conventional medicine as our approach but the high success rate of our treatments for an achilles tendon injury that are directed at treating the tendon and not the bone prove otherwise.
Diagnosis
The diagnosis of achilles tendon injury and heel pain is usually made by the doctor’s clinical exam. However, diagnostic ultrasound or MRI may also be used for a more accurate evaluation.
Causes
- Overuse – This is a common cause for injuries sustained to the achilles tendon. If you overdo it without gradually increasing the activity so your body has time to recover this can be a problem.
- Types of activities – Some activities may make you more susceptible to achilles injury and heel pain. This would include running up and down hills, or any activity where impact or jumping is involved.
- Age – As we get older it is thought that the tendon can become weaker. When this happens the tendon gradually starts breaking down.
- Foot type – Improper foot structure and biomechanics may also play a role. An example is a foot that over pronates, flattens, which may cause more pulling on the tendon. A high arch foot may allow the heel bone to rub against the Achilles tendon.
- Weight – Excessive weight can put excessive load and stress on the tendon.
Prevention
- Shoe gear – Avoid wearing shoes when your active that are broken down. The lack of support may lead to heel pain or Achilles’ tendonitis.
- Heel lifts – If your just beginning to experience pain using a heel lift can take some of the stress off the tendon.
- Changing activities – Consider backing off activities or changing the activity to one that puts less demand on the tendon.
- Stretching – This may also be important both before and especially after activity.
- Anti-inflammatories – taking anti-inflammatories short term may also be useful but long-term use should be avoided as they may have a negative effect on your bodies natural healing processes.

Treatments
Treatments that your doctor may recommend can include resting the area and sometimes immobilizing the area in a walking boot. Physical therapy along with heel pain stretches may also be considered. Also, anti-inflammatories may also be suggested. These treatments can work in the early stages but if the problem is more severe or chronic maybe band aid approaches.
The top four treatments we offer that get at the root cause of the problem. It may not be tendonitis!
- Regenerative medicine – new terminology Achilles TENDONOSIS
The use of stem cell treatments for over the past decade have proven to be phenomenally successful. The new way of thinking about the Achilles tendon and heel pain is that the problem has more to do with the tendon breaking down and having small, microscopic tears then being inflamed. This is called tendinosis. That is why the use of regenerative medicine make more sense. It’s used to repair damaged tissue rather than treat inflammation which may not be present. - Orthotics – The myth of the tight Achilles tendon
Orthotics are commonly used and have a high success rate, why? We know that with every step you take your heel bone rolls from side to side. This motion is thought to put more pulling on the tendon along its length and where it attaches to the heel bone. A custom made orthotic greatly reduces this motion and often eliminates the problem. This goes against the conventional thought. Yes, the pain can be from a tight Achilles but from our experience its less likely than previously thought. - Shockwave – Shockwave is also a treatment that has been successful. Shockwave is similar lithotripsy where sound waves are used to break up kidney stones. This type of treatment sends powerful sound waves in the Achilles tendon area and traumatizes the tendon, but this stimulates your body to send more cellular components to the area that help repair the tendon. This has also shown quite significant relief for patients with this issue.
- Accelerated Laser Pain Therapy – Laser works on a cellular level helping the mitochondria of the tendon tissue repair the tendon. The mitochondria is the area of each cell that creates energy and is responsible for cellular repair.
If the above options fail, surgery may be considered to treat the injury.
Surgery can also be effective but is exceedingly rare as the approach we with orthotics, regenerative medicine, shockwave and laser as options is highly successful at getting you back to full activity.
So if you find yourself dealing with this, understand that you can start out by treating on your own by the suggestions offered in this blog. But the longer this goes on, it’s more important to seek professional attention to ensure that you’re having this treated aggressively. There is a solution for your Achilles tendon heel pain. It’s important that you have consultation with somebody that is proficient providing the treatments we’ve recommended for injuries of this type. If your getting nowhere and feeling frustrated with your present situation please feel free to contact and we’ll help you to evaluate if our approach is appropriate for you.



