
So, you injured your ankle, and you are wondering if it is a sprained ankle vs a broken ankle. Injuring your ankle is a common occurrence, whether during sports or everyday activities. Both ankle sprains and fractures can lead to pain and swelling, affecting the ankle joint and overall mobility. This blog aims to differentiate between an ankle sprain and an ankle fracture, discussing symptoms, treatment options, and recovery times to help individuals understand whether they are dealing with a sprained or broken ankle.
What is an Ankle Sprain?
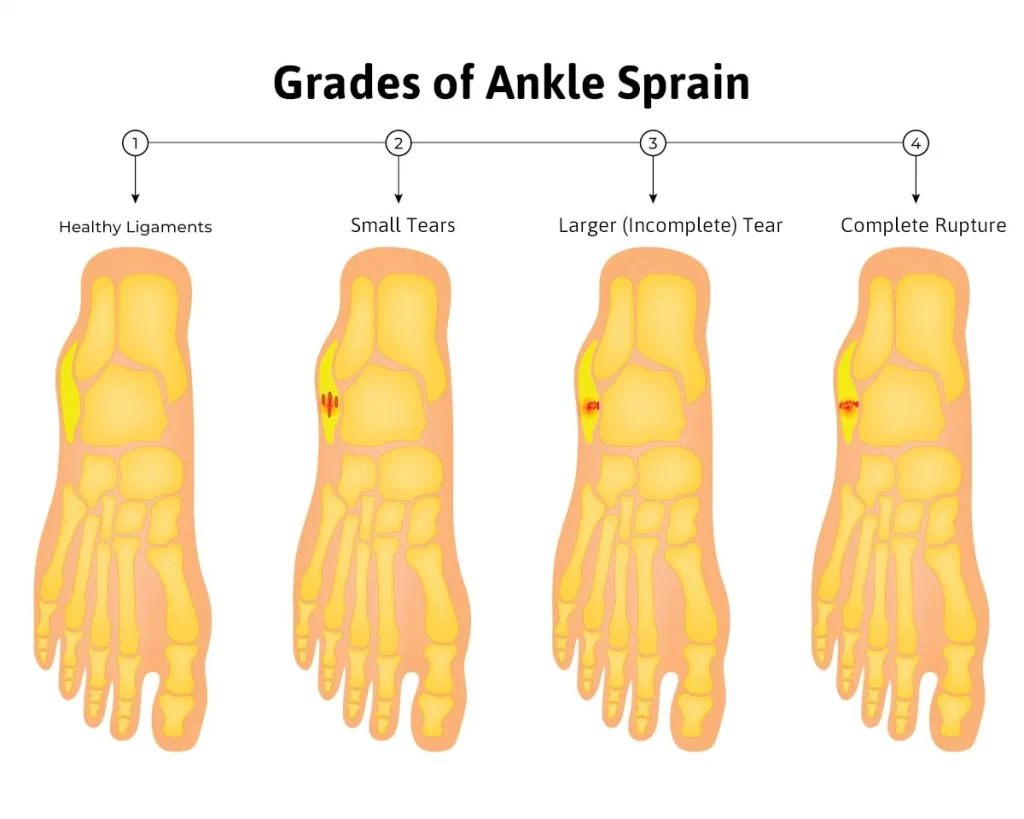
An ankle sprain occurs when the ligaments surrounding the ankle joint are stretched or torn. The ligaments that surround your ankle are important for stabilizing the ankle joint. This common ankle injury often happens when the foot twists or rolls awkwardly during activities. The severity of the injury can vary, with grade I being a mild stretch, while grade III involves a complete tear of the ligaments. When a grade III occurs, aggressive treatment is necessary because the long-term consequence can be a more unstable ankle. Common causes include sports activities and uneven surfaces. Knowing how to identify a sprain can help in seeking medical attention promptly.
Symptoms of Ankle Sprain
Symptoms of a sprained ankle often include pain and swelling around the affected area. Individuals may experience limited range of motion, making it difficult to bear weight on the injured foot and ankle. Bruising may also develop as blood vessels break. Understanding these symptoms can help individuals determine whether they should seek medical attention for further assessment.
What is an Ankle Fracture?
An ankle fracture refers to a break in one or more ankle bones, often resulting from high-impact activities or falls. When you injure your ankle severely, you may hear a cracking sound, indicating a potential fracture. The types of fractures can be classified as stable, where the bone remains in place, or unstable, where the bone may shift. Recognizing the signs of a broken ankle is crucial for appropriate treatment.
Symptoms of Ankle Fracture
Common symptoms of an ankle fracture include intense pain and swelling around the ankle bone. Individuals may notice deformity in severe cases, and there may be difficulty bearing weight on the affected foot and ankle. In some instances, bruising may also occur. If these symptoms are present, it’s imperative to undergo physical exams and imaging tests to confirm the diagnosis. Remember: just because you can walk on the foot or ankle, does not mean it is not broken.
Diagnostic Procedures for sprained ankle vs broken ankle
Both ankle sprains and fractures are diagnosed through physical exams and imaging tests, such as X-rays or MRIs. X-rays are used to evaluate the bones of the ankle and MRI is used to evaluate the tendons and ligaments. These procedures help determine the extent of the injury and whether surgical intervention is necessary. Accurate diagnosis is essential for effective treatment, ensuring that individuals receive the appropriate care for their ankle injury.
Treatment Options for Ankle Sprain
Treatment for ankle sprains primarily involves the RICE method: rest, ice, compression, and elevation. This approach helps reduce pain and swelling while promoting healing. Over-the-counter pain relief medications, such as NSAIDs, can also be effective. In more severe cases, physical therapy may be required to restore range of motion and strengthen the ankle joint. Individuals should monitor their symptoms and seek medical attention if they do not improve.
Treatment Options for Ankle Fractures
For ankle fractures, treatment options depend on the type and severity of the break. Non-surgical options may include casting or immobilization to allow the broken ankle to heal. However, unstable fractures often require surgical intervention, where screws or plates may be used to secure the bones. Follow-up care is crucial to monitor the healing process and incorporate physical therapy to regain strength and mobility.
Recovery and Rehabilitation
Recovery times for ankle sprains typically vary from a few days to several weeks, while broken ankles may take longer, often requiring several months for full recovery. Rehabilitation exercises are vital for both types of injuries to restore strength and range of motion. Failing to properly rehabilitate can lead to long-term complications, emphasizing the importance of adhering to a structured recovery plan.
Long-term considerations for an ankle sprain versus a broken ankle
Ankle Sprains:
When ankle sprains are chronic or you have a grade III that was treated inappropriately, this can lead to chronic ankle instability. A foot specialist may recommend the following:
- Custom-made orthotics: Custom-made orthotics can help reduce the risk of ankle sprains as it always gives the foot and body the feedback as to the positioning of the foot
- Surgery: There are procedures that can reinforce an ankle joint that is unstable by utilizing tendons in the adjacent area or ligaments to help support the ankle better.
Ankle Fractures:
When an ankle fracture occurs, there could be greater incidence of arthritis in the ankle joint in your lifetime. This is because the alignment of the bones that form the joint may be less than perfect. This can cause earlier wear and tear of the cartilage on the joint.
Custom-made orthotics: this may help slow down the degenerative joint disease
Surgery:
- Ankle-scope surgery if there is inflammation of the joint or when the DJD is in its early stages, cleaning the joint out by using ankle arthroscopy can be very useful.
- Joint denervation surgery – this procedure is not well-known, but we have had great success using this technique to avoid or delay the need for an ankle replacement surgery or ankle fusion surgery. The surgery involves cutting specific nerve branches and burying the nerve in the muscle in the lower leg. This type of procedure blocks messages going to the brain signaling the pain from the arthritic joint. These nerves do not supply muscles, so your muscular strength remains intact while greatly eliminating the pain. There is minimal layup after surgery, patients are ambulating within a week.
- Ankle fusion/replacement surgery – these surgeries are the last resort if your ankle sprain has led to eventual ankle arthritis. There is significantly longer recovery period with these procedures.
Conclusion
In summary, understanding the differences between ‘sprained ankle vs broken ankle’ can be crucial for effective treatment. If you suspect an ankle injury, especially if you hear a cracking sound or experience severe pain and swelling, it’s vital to seek medical attention. Proper diagnosis and treatment can ensure a full recovery, allowing individuals to return to their normal activities without the risk of re-injury.
Frequently Asked Questions (FAQs)
1. What are the key differences between a sprained ankle and a broken ankle?
A sprained ankle involves the stretching or tearing of ligaments, while a broken ankle refers to a fracture in one or more bones in the ankle. The severity of pain and the type of injury are typically the distinguishing factors.
2. How can I tell if my ankle is sprained or broken?
Symptoms of a sprain include swelling, bruising, and pain, often without an obvious deformity. A broken ankle usually presents with more intense pain, swelling, difficulty moving the foot, and may include visible deformities or a crackling sound at the time of injury.
3. What are the treatment options for a sprained ankle vs a broken ankle?
A sprained ankle typically requires rest, ice, compression, and elevation (R.I.C.E.), along with possible physical therapy. A broken ankle may require a cast, splint, or even surgery, depending on the severity of the fracture.
4. How long does it take to recover from a sprained ankle compared to a broken ankle?
Recovery from a sprained ankle usually takes a few weeks to a few months, depending on the severity. A broken ankle often requires a longer recovery period, typically 6 to 8 weeks or more, and may involve rehabilitation.
5. Can I walk on a sprained ankle or broken ankle?
Walking on a sprained ankle is generally possible but should be avoided to prevent further injury. Walking on a broken ankle, however, is not recommended, and weight-bearing should be minimized until properly treated by a healthcare professional.




