
Feet are very important for daily function. Whether you are an active runner or like to go on walks for exercise, arthritis pain on the top of your foot can be an issue. The foot is very complex and we know that approximately one-quarter of all the bones in your body are in your feet. Halfway between the ball of the foot by the big toe and where you bear weight and the back of your foot whereby the ankle joint is the midfoot. There are multiple bones in this area that are cube shaped and comprise the arch. It’s a common area to get arthritis in the foot and ankle. These are the affected joints that may cause pain on the top of your foot commonly referred to as midfoot arthritis.
What are the common symptoms?
- A boney prominence in this area is associated with the arthritic joint.
The prominence may rub against your shoe and cause pain.
There may also be numbness, burning or tingling in the same area because the bone spurs are rubbing against nerves beneath the skin. - Dull pain in the morning when you first bear weight.
There may be pain and swelling on the top of the foot. After a few minutes of walking the pain may subside.
Over time this pain may be more severe and prolonged hurting with every step you take
What are the causes of pain on the top of the foot?
The number one problem may be foot mechanics causing more wear and tear on these joints. This type of arthritis is called osteoarthritis. Some feet may be more prone to this issue. Therefore, you are born with the foot biomechanics that might make you more likely to get the problem. Oftentimes a foot type may put more forces through the inner side of the foot by the first and second toe joints. This will cause more stress at the two or three joints in the midfoot associated with these joints in the ball of your foot.
- Trauma- there may be a history of trauma to the area. There may have been an old fracture of partial dislocation or sprain in the foot that now years later will create arthritis and pain.
- Rheumatoid arthritis- pain from arthritis caused by autoimmune disorders such as rheumatoid arthritis.
What you can do for arthritis on top of foot?
- You may need to get a larger shoe or one that is made up of softer material, so it does not rub against the boney spurs.
- Get a stiffer soled shoe- if you’re getting dull pain in the area when you first bear weight in the morning this is a sign of joint arthritis so more support is critical.
- Over the counter arch supports- using an over-the-counter arch support may also be helpful. This can add support to the shoes you have. In the elderly using devices such as a cane or walker may become necessary.
- Choose different activities- If you run consider switching to hiking as this may cause less stress on the joints. You may also consider biking or swimming.
- Lose weight- If you are overweight losing weight will put less stress through the joints and may reduce your pain.
- Medications- consider using nonsteroidal anti-inflammatory drugs NSAIDS. These anti-inflammatory drugs may help with the pain but don’t correct the problem and long-term use may not be good for the joints.
- Supplements and intermittent fasting – this may help reduce inflammation and pain.
What your podiatrist can do?
- Orthotics – this is a common type of treatment recommended especially if you’re getting pain from the joints in your midfoot as this is an indicator of arthritis and more support and dramatically reduce your pain. This process involves getting a non-weight bearing digital scan of your foot so that an orthotic can be made to more accurately support your foot.
- Cortisone injections – These may be helpful if there is nerve damage from the boney spur irritating nerves on the top of the foot.
- Laser treatments – This may also be an option if nerve pain is an issue. Our MLS therapy laser is quick to provide relief with no downtime in comparison to surgery.
- Surgery – Surgery to remove the boney spur may be recommended in some situations where there is minimal joint pain but simply pain from the boney prominence.
Treatments for Joint Pain from Foot Arthritis
As the problem progresses what was once simply a painful bump on the top of the foot may now become pain from the joint that the spur formation is associated with. Then joint pain can become very severe in this area. Fusion of the joint has always been the go-to surgical option. This may involve removing the joint or joints and then using plates staples or bone screws to fuse the joint. It can be successful but there are risks and the lay-up period is weeks of non-weight bearing.
Arthritis Pain on the Top of the Foot: Avoiding Joint Fusion Surgery
Arthritis in the midfoot, also known as midfoot arthritis, is a common condition that can cause significant pain and limit mobility. Many individuals with this condition experience discomfort on the top of the foot, often exacerbated by walking, standing, or wearing certain types of footwear. While joint fusion surgery is a traditional option for treating severe cases, several non-surgical treatments are now available that may help alleviate pain and restore function without the need for invasive procedures.
Surgical Options
When non-surgical treatments fail to provide sufficient relief, surgery may be necessary to restore function and alleviate chronic pain. Traditional joint fusion surgery, also known as arthrodesis, is a common surgical approach, but other techniques may be considered depending on the severity of the arthritis.
Joint Fusion (Arthrodesis)
Arthrodesis involves permanently fusing the affected bones together to eliminate movement in the arthritic joint, reducing pain. While this procedure is effective, it does limit flexibility in the foot and may increase stress on surrounding joints over time. Recovery typically includes a period of immobilization followed by physical therapy.
Joint Resurfacing or Cartilage Repair
For patients with less severe arthritis, procedures that focus on preserving joint function may be an option:
- Cartilage Transplantation: If the damage is localized, healthy cartilage from another part of the body can be transplanted into the affected area.
- Osteotomy: A surgical realignment of bones to redistribute pressure and alleviate pain without completely fusing the joint.
These alternative surgical procedures can help maintain more natural movement in the foot while still addressing the pain and instability caused by arthritis.
Non-Surgical Treatment Options
For those seeking to manage arthritis pain in the top of the foot without undergoing surgery, various non-invasive and minimally invasive treatments can offer relief. These include:
Regenerative Medicine Treatments
Regenerative medicine is a groundbreaking approach that focuses on harnessing the body’s natural healing processes to repair and regenerate damaged tissues. The following regenerative treatments have shown promise in treating midfoot arthritis:
- Platelet-Rich Plasma (PRP) Therapy: This treatment involves extracting a patient’s blood, concentrating the platelets, and injecting them into the affected area. PRP contains growth factors that stimulate healing and reduce inflammation.
- Stem Cell Therapy: Stem cells, typically derived from a patient’s bone marrow or adipose tissue, are injected into the arthritic joint to promote tissue repair and reduce pain.
- Prolotherapy: A series of dextrose-based injections that stimulate the body’s natural healing response to strengthen and repair the weakened ligaments and joints.
These treatments can help improve joint function, reduce pain, and potentially slow down the progression of arthritis.
Joint Denervation
Joint denervation is an innovative technique that targets the nerves responsible for transmitting pain signals from the arthritic joint. By selectively disrupting these nerve signals, patients can experience significant pain relief without altering the structure of the foot.
- Radiofrequency Ablation (RFA): This minimally invasive procedure uses heat generated by radio waves to disrupt nerve function, providing long-lasting pain relief.
- Nerve Blocks: Injections of anesthetic agents can temporarily block pain signals and help determine whether denervation might be an effective long-term solution.
This approach is particularly beneficial for individuals who are not candidates for surgery or who prefer a treatment that does not involve altering the joint itself.
Choosing the Right Treatment for Arthritis on Top of Foot
Determining the best treatment option depends on the severity of the arthritis, the patient’s activity level, and overall health goals. While surgical interventions remain a viable solution for severe cases, non-surgical treatments like regenerative medicine and joint denervation offer promising alternatives for pain relief and improved mobility.
We do it differently at Anderson Podiatry Center!
- Regenerative medicine treatments – for over 15 years we have been one of the leaders in podiatry using restorative medicine. We currently use placenta or umbilical cord products. These are injected into the involved joints. This allows the opportunity for your body’s natural healing processes to reduce inflammation and trigger increased growth factors to repair resulting in pain relief. We have had great success with this option, and it works well as these are not load bearing joints like a knee. With less load, the repair is thought to be improved. These are done in the office and patients return to normal activities in days.
- Joint denervation – This is a process that involves blocking the pain signals to the brain by removal of a sensory nerve branch. There are four nerves in the lower leg that do not affect muscle strength. Any one of them can be safety removed and will not result in weakness. If a branch is removed, it is buried into muscle and patients are ambulating within days. The success rate has been very good and allows patients to delay and in most cases eliminate the need for joint fusion surgery.
As you can see we have multiple options to get you back to full activities and also feel we are well-versed to reduce the need for joint fusion surgery. View our patient testimonials below and when you are ready to meet with a local foot doctor in Fort Collins, give us a call.
Our foot clinic in Fort Collins or our other podiatric foot care office in Broomfield, Colorado is staffed with compassionate, caring, and experienced staff. We will be glad to provide you with answers for arthritis on top of your foot.
Frequently Asked Questions (FAQ) for Arthritis on Top of Foot
-
- What are the early signs of midfoot arthritis?
Common early signs include pain on the top of the foot, swelling, stiffness, and difficulty walking or wearing certain shoes. - How can regenerative medicine help with midfoot arthritis?
Regenerative treatments like PRP therapy, stem cell therapy, and prolotherapy promote healing, reduce inflammation, and improve joint function without surgery. - Is joint denervation a permanent solution?
Joint denervation can provide long-lasting pain relief, but results may vary. Some patients may require repeat treatments over time. - What are the risks of joint fusion surgery?
Potential risks include loss of flexibility, increased stress on surrounding joints, prolonged recovery time, and possible complications such as infection or improper bone healing. - How do I know which treatment is right for me?
A podiatric specialist can evaluate your condition and recommend the best treatment based on your symptoms, severity of arthritis, and lifestyle. - Can I still be active with midfoot arthritis?
Yes, with proper management, including physical therapy, supportive footwear, and non-surgical treatments, many people with midfoot arthritis can maintain an active lifestyle. - How long does it take to recover from joint fusion surgery?
Recovery can take several months, including immobilization and physical therapy. Full recovery may take up to a year, depending on individual healing rates. - Are there lifestyle changes that can help manage midfoot arthritis?
Yes, maintaining a healthy weight, wearing supportive footwear, and performing low-impact exercises like swimming or cycling can help manage symptoms and reduce stress on the joints.
- What are the early signs of midfoot arthritis?



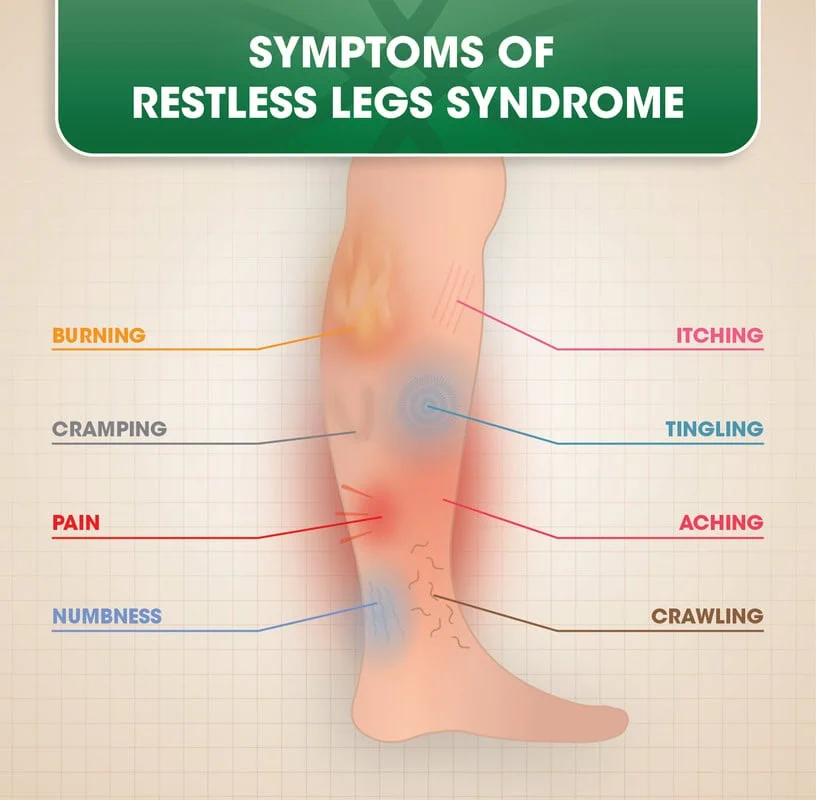 Symptoms are experienced in the legs; particularly from the knee down rather than above. The symptoms can be a combination of cramping, a creepy crawly sensation- like bugs or ants are going on your skin, pain, or jerky legs. However, the most prevalent symptom is an anxious or nervous feeling that makes you want to get up and walk. In fact, most patients have said this is what they have to do during the night.Restless leg syndrome comes on quite slow, and because of this, patients do not realize the severity of the condition. In fact, many in healthcare do not even realize the severity, and their hands are tied because, in many cases, they’re not sure how to help.
Symptoms are experienced in the legs; particularly from the knee down rather than above. The symptoms can be a combination of cramping, a creepy crawly sensation- like bugs or ants are going on your skin, pain, or jerky legs. However, the most prevalent symptom is an anxious or nervous feeling that makes you want to get up and walk. In fact, most patients have said this is what they have to do during the night.Restless leg syndrome comes on quite slow, and because of this, patients do not realize the severity of the condition. In fact, many in healthcare do not even realize the severity, and their hands are tied because, in many cases, they’re not sure how to help.







