Complex regional pain syndrome (CRPS) is a form of chronic pain that could affect the parts of the body, mostly the arm, leg, hand or foot. It is not fully understood what causes complex regional pain syndrome. By reading this blog you should be better informed if you have this condition as early treatment can be very important. Another term that is often used is called reflex sympathetic dystrophy which has similar symptoms but tends to be a more severe state of complex regional pain syndrome.
The signs and symptoms of Complex Regional Pain include the following
- Changes in skin temperature – the affected area may be warmer or cooler.
- Changes in skin color – the skin may be whiter or have a purplish or bluish discoloration.
- Muscle spasms and weakness in severe cases.
- Burning and/or throbbing pain.
- Sensitivity to touch or cold temperatures.
- Decreased ability to move the affected limb.
It is important to note that occasionally CRPS can spread elsewhere in the body including the opposite limb. The symptoms of CRPS may go away on their own but for many the symptoms may persist for months or years and early treatment is most effective to reverse the symptoms.
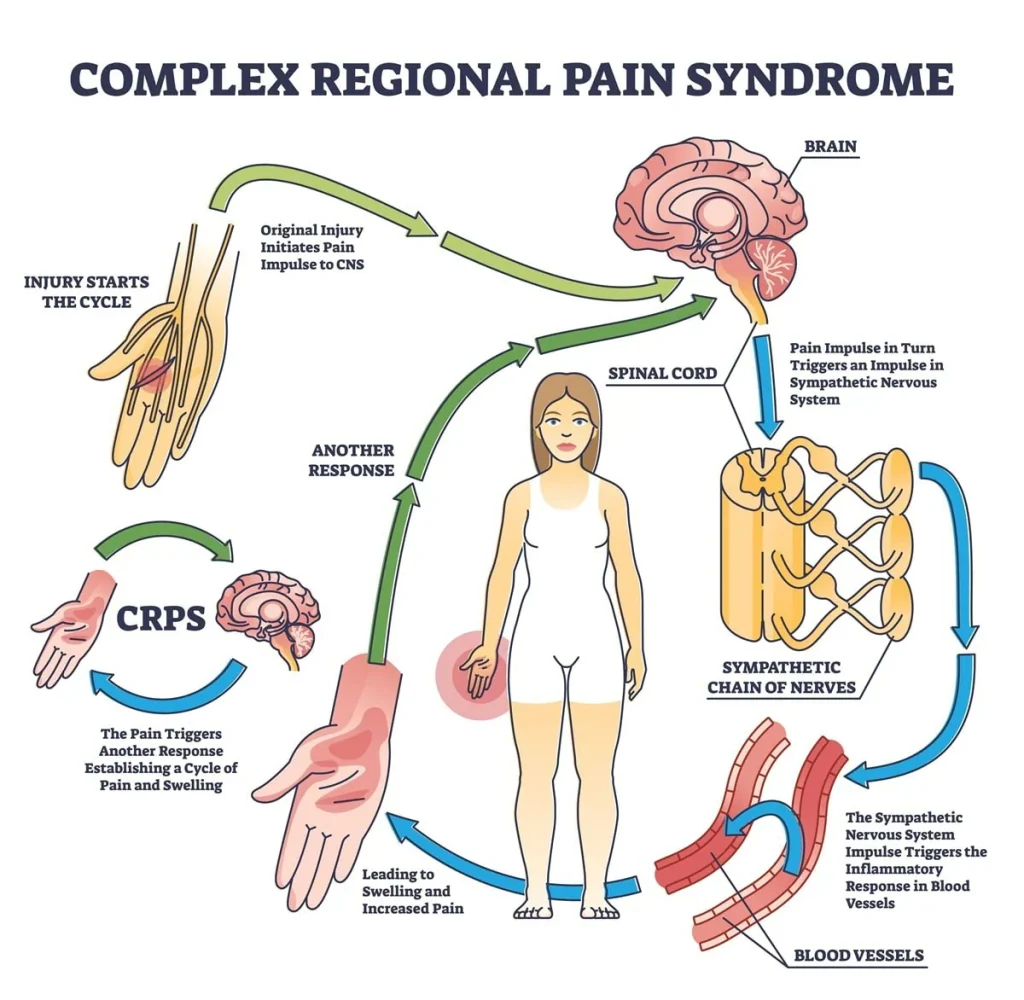
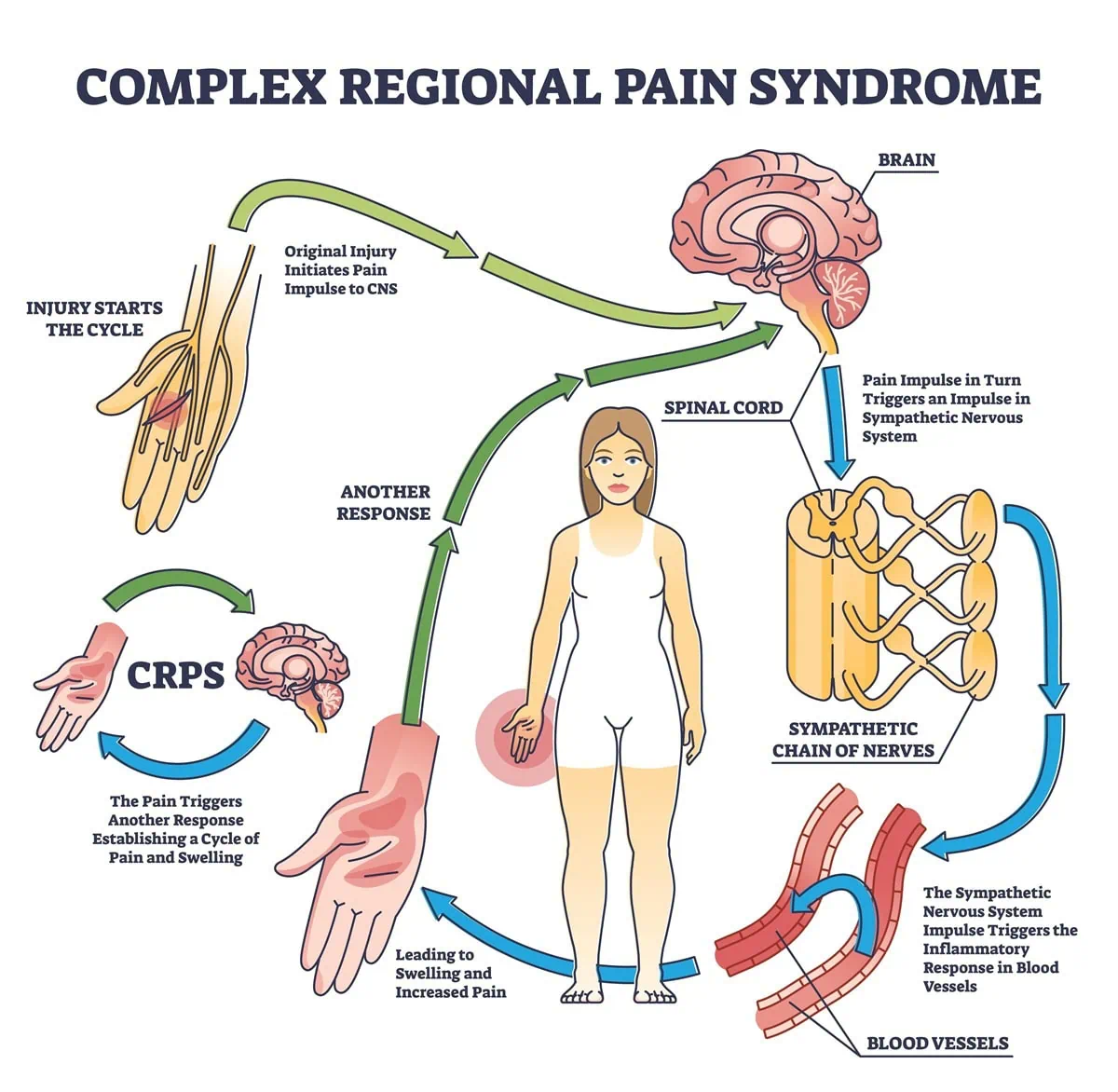
Causes of Complex Regional Pain Syndrome
Conventional Medicine categorizes CRPS into two types:
- Type 1 – this is often referred to as reflex sympathetic dystrophy and may occur after an injury or an illness but there may not be any direct damage to the nerves of the affected area. Most people are thought to be type 1.
- Type 2 – this is often referred to as causalgia. The symptoms of this type are similar to type 1; however, type 2 occurs after a specific nerve injury.
The following are examples of what may cause the symptoms of CRPS. They include a crushing injury, fracture, ankle sprain, heart attack, strokes, and for others, it may be a result of surgery on the hands, feet, or legs. With more chronic CRPS, treatments may be more challenging as it may start to affect the central nervous system also. Whereas in the beginning, it was a localized issue in the lower extremity. The full mechanism between the central and peripheral nervous systems is not well understood as it relates to CRPS.
How do doctors diagnose CRPS?
- Patient’s History – The patient will report an illness, injury, or surgery where symptoms started for many people.
- Specific tests to diagnose CRPS include Ultrasound or Magnetic Resonance Imaging (MRI) which may be used to identify underlying nerve damage.
- EMG may also be used for testing nerve function.
Conventional Treatment Options
For many, the treatment of CRPS involves seeing a doctor who specializes in pain management, and the pain management doctors may use the following treatments.
- Physical Therapy/Occupational Therapy
- Psychological and Behavioral Therapy
- Medications – this can include nonsteroidal anti-inflammatory drugs, anti-depressant drugs that may be used, and also anti-seizure drugs such as gabapentin and pregabalin. These medications are usually prescribed to treat CRPS.
- Narcotics – If other medications fail, narcotics may be used and carefully monitored by the prescribing doctor.
- Topicals – topical analgesic creams can be used such as lidocaine.
- For severe symptoms, the use of spinal cord stimulation.
- Sympathetic nerve blocks – these blocks involve injections to the lumbar area of the back which can offer pain relief but is usually temporary.
- IV ketamine infusions – this is another treatment option.
Things that you can do at Home
- Exercising on a daily basis is important to move the affected body part and it may help repair the damaged nerves.
- If there is swelling present, compression stockings may also help.
- If there is a swelling in the limb, elevation while resting may also be helpful.
The game-changing approach that peripheral nerve surgeons are using to discover the root cause and reverse CRPS.
The Non-conventional Treatment Options
Demystifying the cause of Complex Regional Pain Syndrome: Why you should consider consulting with a peripheral nerve surgeon
With the advancement of the knowledge of the peripheral nerve system in the lower extremities, a subspeciality of doctors has been created that specializes in the evaluation and treatment of peripheral nerve disorders including neuropathy, restless legs, and chronic pain. From our knowledge and experience, we are now able to reverse the symptoms of CRPS by evaluating and treating the injured nerve. This has helped many patients avoid the need for spinal cord stimulators and has allowed others to get off narcotics.
What are the options a peripheral nerve surgeon would offer?
- Injections – Injections may be used in the early stages to reverse the symptoms of the damaged nerve but are also helpful in identifying which nerve branches are damaged.
- Laser Treatments and Electrical Stimulation Treatments – These treatment modalities can be used if in mild cases.
- Surgery– Surgery may involve the removal of the damaged nerve branch and also burying the nerve in the muscle to prevent regrowth.
The goal of a peripheral nerve surgeon is to discover the specific nerve that has been damaged and address treatment locally in the foot or leg. Thus, eliminating the need for medication or spinal cord stimulators for many. If you would like to learn more about these options, please consider visiting https://www.aens.us/aens/default.asp
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.

 What is Chronic Pain?
What is Chronic Pain? Chronic Pain and Your Personality
Chronic Pain and Your Personality
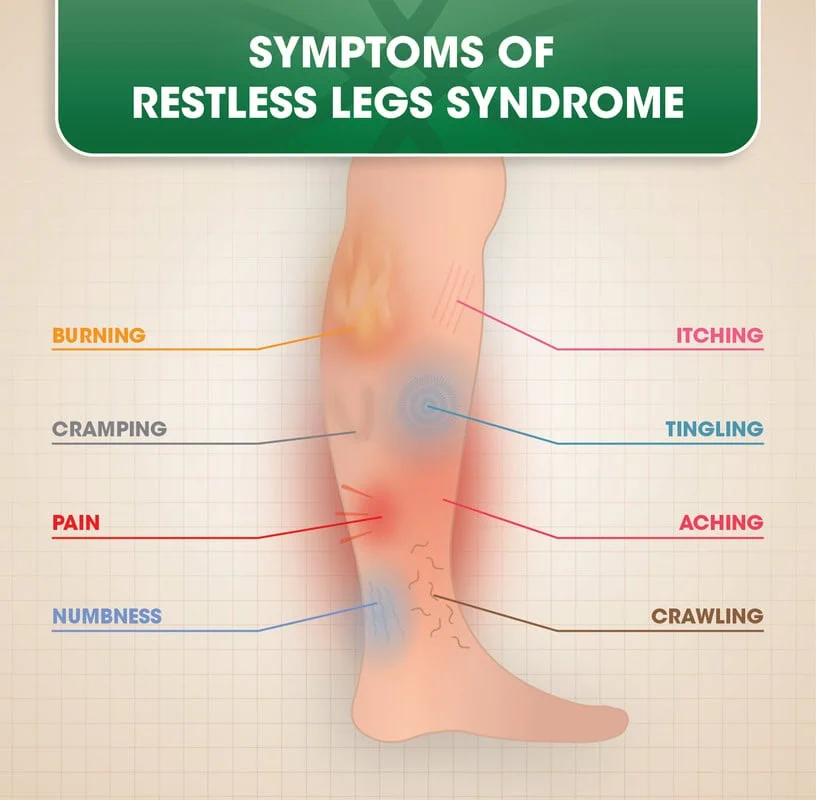 Symptoms are experienced in the legs; particularly from the knee down rather than above. The symptoms can be a combination of cramping, a creepy crawly sensation- like bugs or ants are going on your skin, pain, or jerky legs. However, the most prevalent symptom is an anxious or nervous feeling that makes you want to get up and walk. In fact, most patients have said this is what they have to do during the night.Restless leg syndrome comes on quite slow, and because of this, patients do not realize the severity of the condition. In fact, many in healthcare do not even realize the severity, and their hands are tied because, in many cases, they’re not sure how to help.
Symptoms are experienced in the legs; particularly from the knee down rather than above. The symptoms can be a combination of cramping, a creepy crawly sensation- like bugs or ants are going on your skin, pain, or jerky legs. However, the most prevalent symptom is an anxious or nervous feeling that makes you want to get up and walk. In fact, most patients have said this is what they have to do during the night.Restless leg syndrome comes on quite slow, and because of this, patients do not realize the severity of the condition. In fact, many in healthcare do not even realize the severity, and their hands are tied because, in many cases, they’re not sure how to help.







