Do you have questions about diabetic foot care? Read this to know more!
Diabetes can be profoundly serious for your feet. In this blog, I will explain what you need to know about diabetic foot care. But before we get started on a list of things to keep in mind, it’s important to remember three basic principles about your feet. Understanding the following will give you better clarity regarding your diabetic feet and what’s important to consider.
Three ways diabetes affects your feet.
- The nervous system – If you have diabetes there is a 50-70 percent chance you will have neuropathy. Diabetes can cause nerve damage especially in the feet and lower extremity. This will result in the symptoms of burning tingling and numbness in the feet. Because of numbness problems such corns and calluses may not be felt. At first the idea of numbness in the feet may not seem that bad because it might prevent you from feeling pain but that’s where the problem lies. This prevents the warning signs of pain that can be associated with an ingrown nail, a cut or blister. Quite common and serious issues occur with callouses on the bottom of the foot. With no pain the callous may eventually break down the skin causing an ulcer. Once the skin has broken open from the ulcer an infection is likely, and this can eventually get into bone. Once this occurs an amputation is more likely,so without the nervous system giving a warning in the form of pain problems such as corns, calluses, blisters and ingrown nails become more serious.
- Circulatory system – It’s also known with diabetes that you have a higher propensity to have decreased blood flow to the lower extremity, especially the feet. When this happens, if there is any kind of cut or problem with the foot it may be harder to heal properly. It should also be emphasized that smoking combined with diabetes should be avoided. There is a many fold increase of circulatory complications with people who smoke. If a toe is injured with a cut and develops an ulceration, a dark area of the skin in this area could be an indication of gangrene and should be evaluated immediately.
- Foot Deformities – Any type of foot problems such as a bunion or a hammer toe can create any irritation where the bony prominence will rub against shoe gear. This too can cause a problem because this can lead to a breakdown in the skin in the form of a callous or a corn that can eventually cause a foot ulcer. Properly fitted shoes are especially important. If the deformity is severe and difficult to accommodate in shoe gear, surgical correction may be considered by the podiatrist after appropriate workup, to ensure adequate blood flow is present for healing. Better to correct earlier then later in some situations as the circulation could become compromised enough later in the life to where surgery would be too risky.
General guidelines to follow
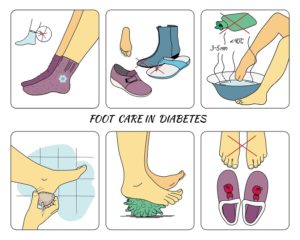
By following these tips, you can do a lot to take better care of your diabetic feet.
- Be sure that you bathe your feet daily. Be careful to dry your feet especially between the toes after you are done.
- It’s a good idea to inspect your feet every day. You may need to use a mirror to look throughout the foot on the top and on the bottom. Also in between the toes for any types of cracks or cuts that may be there.
- Make sure to avoid walking barefoot. This is obviously a problem if you step on a foreign body or a cut.
- Make sure that you test water with your hand before putting your foot in warm water such as a hot tub or a bath.
- Use appropriate shoe gear and socks.
- Make sure that you attributed nails and not dig in on the sides. Try to cut them somewhat straight across as if you don’t this could cause an ingrown nail.
- Make sure that you control your diabetes well by controlling your blood sugar levels.
- Make sure that you see your podiatrist on a regular basis. Some will recommend coming in every two to four months just for a general foot inspection.
- With diabetes your feet may become drier, and this can cause cracking of the skin. So be sure to keep your skin moisturized.
- Make sure that you have your foot checked by a professional, especially if you are getting a corn or a callus that could be problematic and painful.
- Never treat corn and calluses yourself. Over the counter products that are sold frequently have acids in them that eat away at the corn or callus. This is too risky to use in the diabetic foot.
- Wear socks to bed if your feet are cold at night.
Diet Tips
To stop or delay nerve damage avoid carbohydrates and sugars. Make sure to have a diet that includes vegetables, fruits and protein. Also, a diet that includes fat is important as nerves need fat for proper function. Make sure it’s healthy fat such as grass-fed butter. A daily habit I have is to add grass fed butter to my coffee along with cinnamon. This avoids unhealthy additions to the coffee such as sugar or artificial creamers. The fat also satisfies your hunger so that you’re less likely to want to eat. A great book to use as a reference is Sugar Crush written by a colleague of mine Dr. Richard Jacoby.
Following these general guidelines should help you protect your feet from a dangerous situation that could occur when you have diabetes. Educating yourself is key when you want to prevent any serious problems.













