Diabetes is a common problem that is affecting more people worldwide and Charcot foot is associated with the diabetic foot. It may be one of the most overlooked problems for not only the patients but healthcare providers in the diabetic population. Charcot foot can result in foot deformities which can be debilitating from a functional standpoint but also put you more at risk of amputation. It has been estimated that two percent of diabetics have a Charcot foot. The percentage is low but the risk of not knowing about it can put you at risk as early diagnosis and intervention are important. So, what is a Charcot foot, and what causes it?
Description
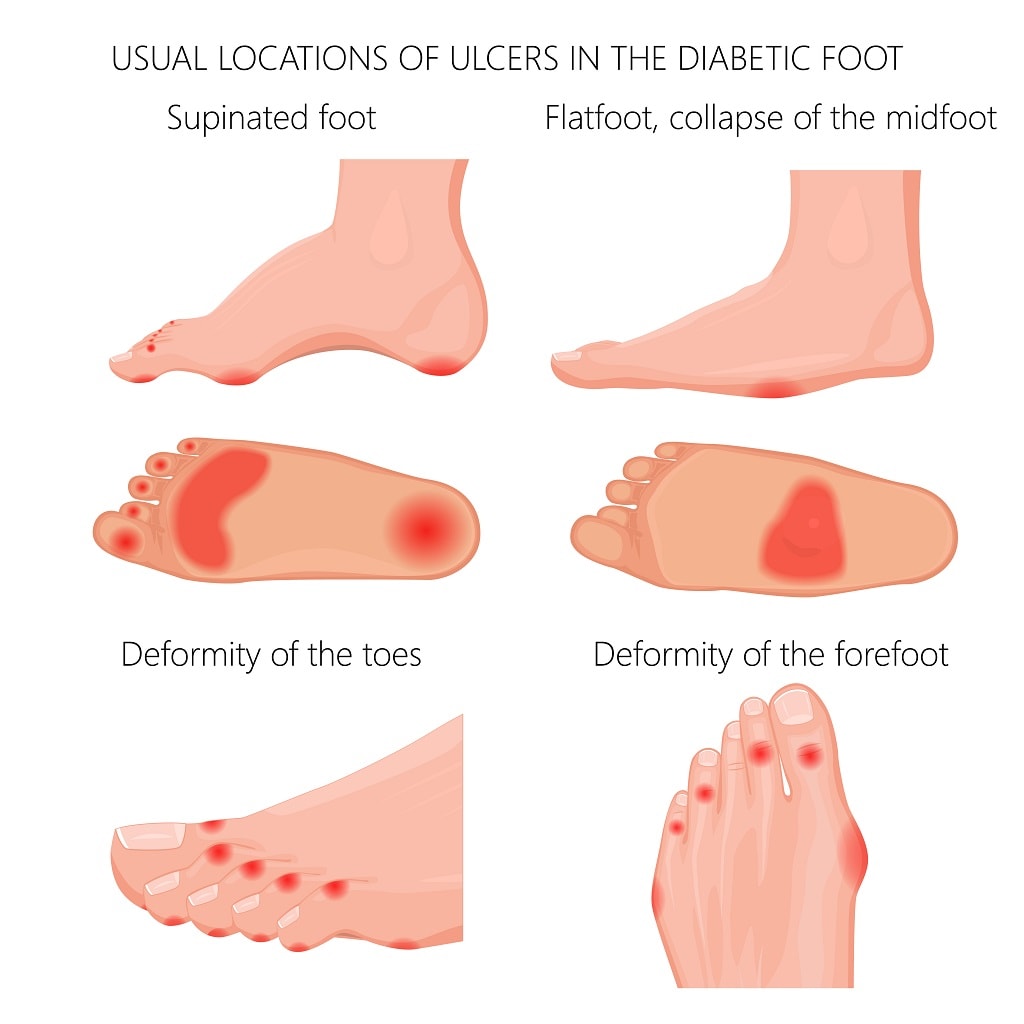
A Charcot foot can result in the breakdown of the foot. There may be multiple fractures that occur primarily in the midfoot region. The result can be a foot that becomes very flat. So flat that it may be referred to as a rocker-bottom foot. This means there is no arch but instead where the arch used to be there can be boney prominences associated with the deformity. This causes excessive pressure on the soft tissues and skin and eventual risk of callouses which can then ulcerate and lead to infection. So how did this come about? What can increase your risk? It can be from poor control of your diabetes, a broken bone, or an injury to the foot and ankle To understand how you get a Charcot foot and why this puts you at risk we need to discuss diabetes and its effect on the nervous system and the arterial system.
Nervous system
It is common for people with diabetes to have neuropathy. Approximately 50-70 percent of diabetics have this condition. This will cause burning tingling and numbness in the foot. The numbness is what puts the diabetic foot at risk because of what we refer to as a protective sensation. If you have numbness, you may not feel what normally would have been a painful callous for instance. The callous then breaks the skin down and this leads to an infection. What is happening in the Charcot foot is the damage to the nerve’s effects blood flow to the foot. The damage to the nerves may occur in the autonomic nervous system which regulates blood flow. When the nerves are damaged the small nerve branches that regulate blood flow by constricting blood flow no longer work and the arteries dilate. This causes an increased amount of blood in the foot. This then results in the diminishment of calcium in the bone and the bones of the foot become weaker and fractures occur. The bones and joints that support the foot collapse causing various deformities which are referred to as a Charcot foot. Circulatory system
Circulatory system
The arterial blood flow that takes blood from the heart down to the foot is affected in the diabetic state. When it occurs, it’s referred to as arteriosclerosis and tends to involve the smaller arteries in the lower legs and into the foot.
What are the symptoms of a Charcot foot?
The primary symptoms can be a hot red swollen foot. A Charcot foot is commonly misdiagnosed as being infected or a gouty attack. Both of these can also cause redness and warmth in the foot. Because of neuropathy being present the patient may experience little to no pain and that’s what makes this dangerous.
How is Diabetic Charcot Foot diagnosed?
Often a diagnosis is arrived at by exclusion of other problems such as infection or gout. X-rays are also important as fractures may be seen and evidence of flattening of the arch. The foot that is affected may begin to have a flatter appearance compared to the opposite foot.
What are the treatments options for someone with Diabetic Charcot Foot?
When diagnosed early it’s important to have the patient immobilized and be non-weight bearing to reduce the breakdown of the foot. Because the foot may have small fractures and the stability has been compromised casting the foot and remaining non-weight bearing is the standard treatment. This will lessen the amount of deformity that occurs and protect the fractures from getting worse. With proper treatment, the number of foot deformities that occur can be greatly reduced. The amount of time for casting may vary but can be a minimum of two months or more in many cases.
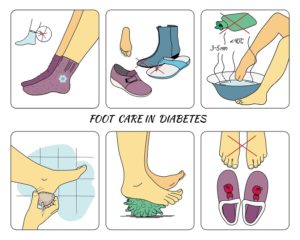
Special shoes and orthotics. Conservative treatment may include orthotics or custom shoes to reduce pressure on soft tissues from the boney pressure points
Surgery – If the Charcot foot is not diagnosed and no treatment is done or it is treated but not early enough then surgery may be necessary to reconstruct the foot. These surgeries are among the most challenging foot procedures and require immobilization and non-weight bearing.
What you need to know – If you are diabetic and your foot feels warm or looks red, think Charcot foot as it may not be an infection! Both can appear the same.
So even though the chances of you getting a Charcot foot are very rare, it’s important that you remember the points covered in this blog. If you or someone you know is diabetic please seek medical attention if you suspect these symptoms as it can help to lessen the chance of amputation.