For many suffering from diabetic peripheral neuropathy, the information in this blog may be the most important you need to know when seeking treatment. We will discuss the basics of diabetic neuropathy and the conventional treatment options. However, you’ll learn how it’s reversible and we will contrast how centralized medicine continues with the same old dogma that you cannot reverse it. So, consider the other option I’ll be explaining. I will explain why I consider myself and my colleagues decentralized doctors, so you’ll better understand why centralized medicine keeps this information from you. You’ll also get access to research to prove my claim.
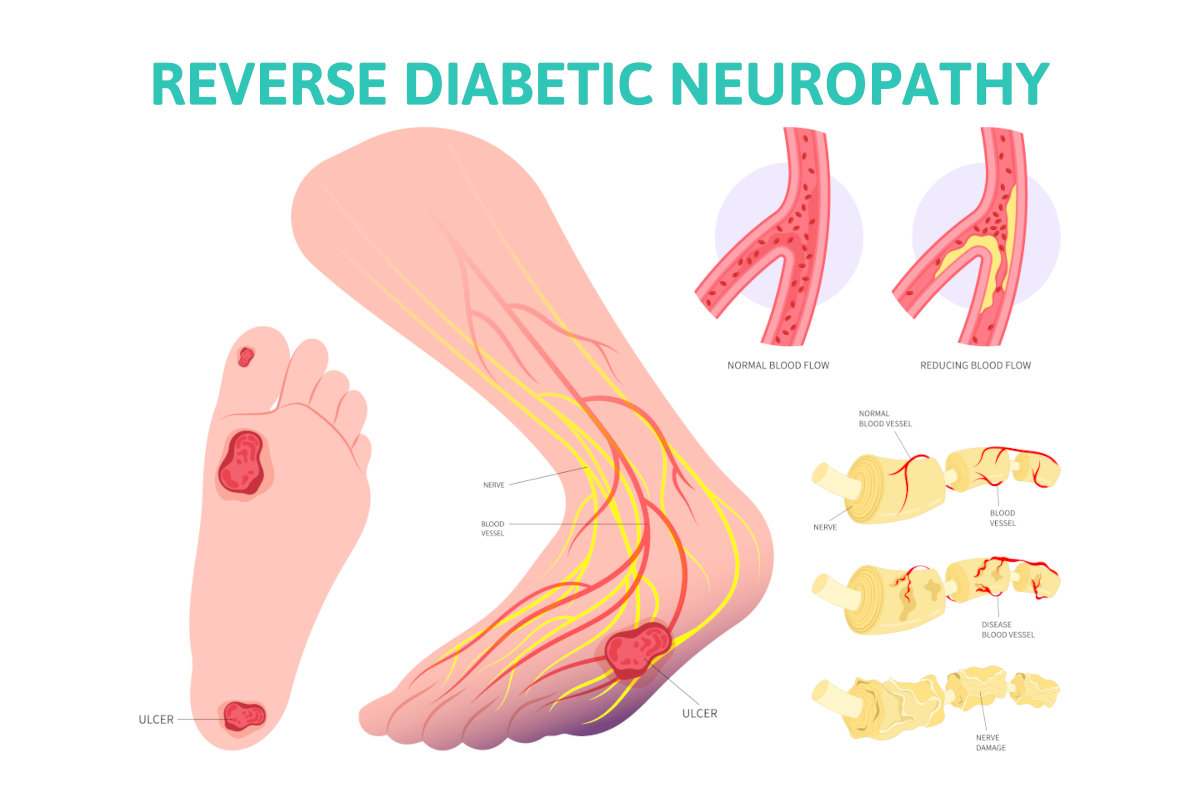
Approximately 50-70 percent of those suffering from diabetes will develop neuropathy. The symptoms of diabetic neuropathy will be burning, tingling numbness, and sometimes weakness in the feet and may extend above the ankles into the lower legs. The challenge is that as you lose sensation it will put you at greater risk of an amputation, the most concerning complication of diabetes.
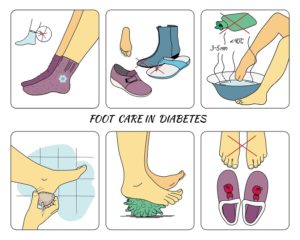
With the nerves that control sensation your ability to feel a sore, like a callous, will be diminished. That callous may become deep, breaking down the skin and resulting in an ulcer. Then an infection may start with infection getting into bone and an amputation of a toe or portion of the foot may be necessary. Because of this risk people with diabetes are more at risk of early death from this amputation risk. The autonomic nervous system may also be damaged with diabetes. This may affect the heart, bladder, sweat glands, and sexual function.
Types of diabetic neuropathy
- Small fiber disease– This is a common type of neuropathy and this term is used to describe nerve damage to the small nerve fibers that lie right beneath the skin. By taking a biopsy of the skin, the number of nerve endings can be counted to see how many are dying. Small fiber disease will cause burning tingling and numbness as the nerve endings die.
- Large fiber disease – This may also occur but is not frequently talked about. This is nerve damage from compression. The compression is coming from nerve tunnels that become too tight. Carpel tunnel syndrome would be an example of this.
- Type one and type two diabetes – You’ll commonly hear these terms and it’s important to know what they mean. Type 2 diabetes is most common and affects people later in life. The pancreas still makes insulin but in smaller amounts. Type 1 diabetes refers to diabetes that starts at a young age and the pancreas does not produce insulin.
Conventional treatments for diabetic neuropathy
Treatments are the following
- Control diabetes – It is thought that controlling your blood sugar levels will be less damaging to the nerves and therefore the progression of neuropathy may be reduced. By controlling risk factors such as too much sugar and carbohydrate intake glucose levels can be better controlled.
- Medications– medications such as Lyrica and Gabapentin are commonly recommended to control the symptoms as they become more severe. These drugs may have a positive effect on the burning tingling and numbness symptoms. In rare instances, narcotics may also be prescribed.
- Medications for controlling blood sugar levels – These can vary depending on the type of diabetes you have and by controlling sugar levels less damage to the nerves may take place.
- Exercise – this may improve blood flow. Also, it may help the body’s metabolism to control high blood sugars and have a positive effect on the health of the nerves. The blood vessels that supply the nerves may be better able to keep the nerves healthy. It will also reduce risk factors such as weight and high blood pressure.
Here’s what you’re being told about your diabetic neuropathy.
It’s not reversible and if you have it it’s from metabolic issues. The high glucose levels are detrimental to the nerves so the primary solution is medication to help with the symptoms. This is the centralized medical recommendation. Most of healthcare has bought into this narrative. It begins in medical schools with training of doctors to prescribe these drugs and also with the millions of dollars spent by big pharma to promote to the public. Understand the centralized concept is that big pharma along with government agencies fund the research that we fund through our taxes and then promote to you and doctors. No wonder that’s all you’re hearing.
The other new option for diabetics with neuropathy
Surgical reversal of your diabetic neuropathy. Yes, surgery can reverse your diabetic neuropathy.
The basics of nerve decompression for diabetic neuropathy.
When your blood sugars are higher than normal, glucose is broken down by another metabolic pathway called the polyol pathway. In this process, a sugar molecule called sorbitol is created. The sorbitol molecule then gets into the peripheral nerves and attracts water to the nerves. As more water is absorbed into the nerve it will swell as much as forty percent. The swelling of the nerve then creates compression on the nerve as it travels through nerve tunnels. This is why carpal tunnel syndrome is much more common in diabetics. This argument has been around for over twenty years. This information is coming from decentralized doctors like me. No drug company has funded my research, it is there to be read by all doctors and the public.
Objective research to prove that diabetic neuropathy is reversible. Me and my team of doctors have published two papers providing objective evidence of diabetic neuropathy. Two attempts were made to present this at the national meeting of the American diabetic association, and we were turned down. I was innocent enough to think we would be accepted with open arms. Obviously, there is another agenda.
The basics of our research. Patients with severe diabetic neuropathy underwent nerve decompression surgery to remove pressure on the nerves in the lower extremity. Intraoperative EMG studies were done before and then immediately after the nerve tunnel had been opened and decompressed. To do the test needle electrodes were placed in the muscle that the nerve supplied to measure how much the nerve caused the muscle to contract before and after the nerve tunnel was opened. Some patients had up to 300 percent change in this number. Again, this is objected data supplied by a machine used to measure nerve function. So, it is indisputable evidence and helps with understanding the relation to finding the right treatment for diabetic neuropathy. Here are the two studies.
Since those two studies were done there is even more research to show that patients undergoing these procedures for treatment of their diabetic neuropathy have significantly reduced the potential for an ampuation. A study by Dr. Zhang in china reports emg nerve testing before and after surgery. 1

Amputation costs to the healthcare system can be a minimum of 80,000 dollars. Besides the monetary price, there is the cost of human life as once a limb is amputated life span is significantly reduced.
So if the centralized medical dogma could be shifted fewer drugs would be sold, fewer patients would need to go to wound care centers where many centralized medical products are used. You’re not hearing the option because if you’re a diabetic patient that is conscientious about your diabetic condition you are consulting with your doctors who manage your condition. Yet they are slow to change and have continued with the medical dogma of centralized medicine. As a peripheral nerve surgeon myself and my colleagues have patients coming to us that refuse to accept the status quo. Sadly, for new concepts to get traction and be fully accepted by the masses it takes a lot of capital.
Doctors have to be monetized so that the services we offer have a positive effect on a company or industry that collaborates with us to move the new concept forward. They win, the doctors win and so do the patients. So this relationship does not exist for doctors that do what me and my colleagues do for the treatment for diabetic neuropathy. As of yet there is no such relationship with an industry with big pockets to promote and further research what we do. Yes, for many the drugs that are used are helpful at reducing the symptoms. However they also allow for the deterioration of the nerves to continue and the risk of amputations go up! If you’d like to learn more about someone in your area who is trained as a peripheral nerve surgeon, please go the Association of Extremity Nerve surgeons website.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.
References
1 Evaluation of the clinical efficacy of multiple lower-extremity nerve decompression in diabetic peripheral neuropathy
Zhang W, Zhong W, Yang M, Shi J, Guowei L, Ma Q. Evaluation of the clinical efficacy of multiple lower-extremity nerve decompression in diabetic peripheral neuropathy. Br J Neurosurg. 2013 Dec;27(6):795-9. doi: 10.3109/02688697.2013.798854. Epub 2013 May 29. PMID: 23713665.
https://pubmed.ncbi.nlm.nih.gov/23713665/

 Opiate Addiction
Opiate Addiction



 What is Chronic Pain?
What is Chronic Pain? Chronic Pain and Your Personality
Chronic Pain and Your Personality



