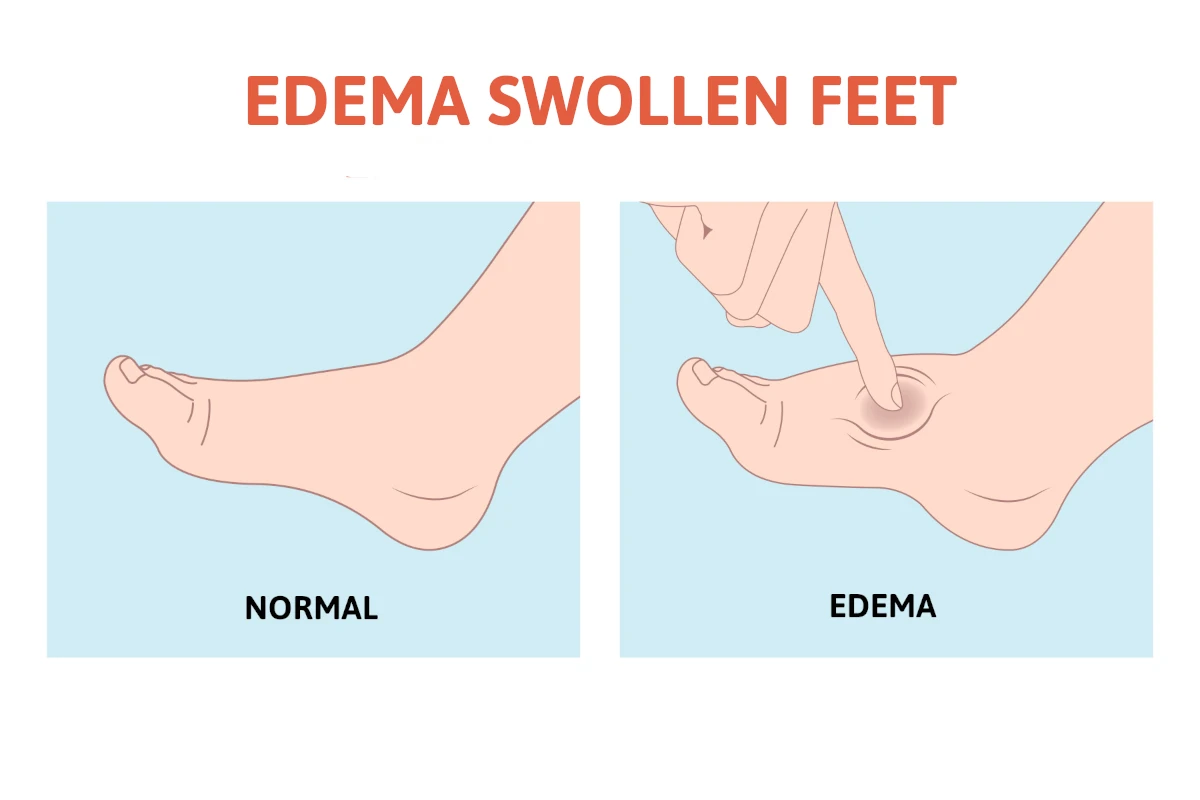
 If you note swelling in the lower extremity, the swelling is commonly called edema. Edema is a problem that can be seen in any body part including the abdomen, and arms but it is most common in the feet and lower extremities. Edema in the legs simply means the accumulation of fluid in the body’s tissues. There can be multiple causes and the older you get, the more likely you may experience edema in the lower extremity. It is more common over the age of 65.
If you note swelling in the lower extremity, the swelling is commonly called edema. Edema is a problem that can be seen in any body part including the abdomen, and arms but it is most common in the feet and lower extremities. Edema in the legs simply means the accumulation of fluid in the body’s tissues. There can be multiple causes and the older you get, the more likely you may experience edema in the lower extremity. It is more common over the age of 65.
What are the symptoms of edema in legs?
- Tightness or uncomfortable feelings – Because of the pressure of the swelling in the legs, they may feel heavy and may cause dull pain.
- Difficulty with walking – The swelling may be significant enough that the heaviness of the edema may increase the weight in the limb and make moving the joints more difficult. Walking may be more difficult because in the legs, and ankles, there may be increased weight from the fluid accumulation in the legs or in the feet and ankles and reduction of motion in the joints.
- Dermatological – The skin may become more stretched and pitted which means when you press on the skin an indentation may remain for a period of seconds. Also, for patients whose swelling is from varicose veins, a dermatological called stasis dermatitis may occur causing a brownish discoloration and itching on the skin.
- Location – Edema does not tend to be in a small swollen area but rather over a larger region.
What causes edema in legs?
The causes of edema can be multiple and can be related to various medical conditions.
- Salt intake – Having too much salt in your diet can cause retention of fluid in the body and this can lead to fluid buildup in the lower extremity.
- Venous disorders – The veins are blood vessels that return blood to the heart after it has traveled to the lower extremity via the arteries. People may have had deep vein thrombosis which is a medical term for blood clot. Afterwards, they may have edema in the lower extremity. During a blood clot, swelling may be an early warning sign that it is occurring and if chest pain is associated with this, consider it a medical emergency and seek immediate treatment.
- Heart failure– Patients with heart failure are also more likely to have edema in the lower extremity and can be an early warning sign of this condition.
- Kidney disease – Kidney disease can also be a cause of edema and may be an early indicator that you may have this problem. If you have swelling in your legs and feet and this is accompanied with difficulty breathing, it would be important to consider kidney disease, call 911.
- Lymph nodes – Lymph nodes are part of the lymphatic system and may facilitate drainage from the lower extremity. Some may suffer from lymphedema which causes generalized swelling of both legs in the lower extremity, and it can make walking difficult, and it may cause tightness in the lower legs.
- Medication – The side effects of some medications can cause swelling, and this can include medications for high blood pressure, estrogen, and testosterone medications, some medications that treat nerve pain, and diabetic medication.
Treatment
Treatment options for edema in legs include the following:
- Monitor your salt intake. If the swelling is mild and you believe you have too much salt intake, one of the first steps is to lower your salt intake in your diet.
- Avoid sitting or standing for long periods of time and instead consider walking or elevating your legs when you’re sitting.’
- Wear a support hose. Support hose can typically be purchased over the counter and create compression on the limb that will help reduce the swelling. It is important to put this on early in the morning before you walk and when your edema is at its lowest.
- Treatment of related medical conditions. When the edema is chronic and more severe, it is very important that you see a healthcare provider to rule out problems such as heart failure, pulmonary (lung) problems, kidney disorders, and problems in the circulatory system including the veins and the lymphatic channels.
Treating the cause of the problem
Once the potential cause of the problem is addressed, sometimes medications to control high blood pressure as an example or surgical procedures to address problems such as varicose veins or lymphedema, the swelling may be improved.
The information in this blog should offer you important information regarding the edema in legs that you might be experiencing. One of the biggest takeaways is that edema can be the first warning sign that you are starting to experience a serious issue such as heart or kidney problems. You should not forget that swelling in the legs accompanied with difficulty breathing should be considered as a medical emergency and can be a sign of a blood clot. A quick emergency evaluation is important. Finally, if your symptoms are more chronic and severe, always err on the side of seeking medical attention.
Swollen, heavy legs from edema? Our specialists offer advanced treatments to reduce discomfort and improve circulation.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.