The sesamoid bones are small pea shaped bones that sit beneath the big toe joint. Where there is pain under your big toe it may be called sesamoiditis pain. Let’s look at why you may be seeking sesamoiditis treatment to resolve a common foot pain.
Sesamoiditis basics – The sesamoid bones are like the kneecap, patella bone. They sit beneath the big toe joint and the great toe, and both are attached to muscles and tendons that help pull the big toe downward. Much like the kneecap they each glide in a groove under the joint. They function to increase the leverage of the muscles of the foot to pull this toe downward. This motion is very important for normal gait while running or walking. You may have heard of the term turf toe, this is associated with the sesamoid bones but may also involve inflammation to the tendons and muscles that attach to the sesamoids.
What are the symptoms of sesamoiditis?
Sesamoiditis pain tends to be very localized beneath the big toe joint in the ball of the foot. You’ll favor your foot tending to avoid putting pressure on the bottom of the great toe. High heels will make the pain worse. You may have swelling associated with it. The pain tends to be deep and dull, and you may notice it the most when you first step down in the morning. Which is why most people try to pass it off as morning stiffness and not seek sesamoiditis treatment.
What is the cause of sesamoiditis?
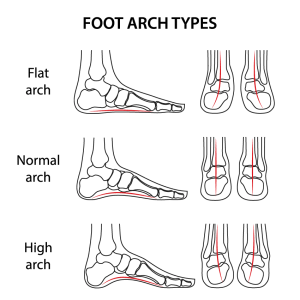
- Foot type – some feet may tend to roll inward referred to as pronation. This would cause more pain to be placed on the ball of the great toe.
- Trauma, sesamoid fractures. You may have fractured the sesamoid bone. You’ll usually be aware of this as a lot of force would be needed to cause a fracture. Landing with a lot of weight on the great toe or severely jamming your great toe upwards may cause a fracture.
- Bunions – A bunion deformity causes the great toe joint to be misaligned. Because of this the seamaids may no longer glide centered in the grooves beneath the metatarsal bone but may now be gliding over centered. This may result in erosion of the cartilage on the ridge that separates the two grooves. Both the cartilage on the seamaid bone and the cartilage on the bottom of the metatarsal breakdown causing octopartite to occur
- Hallux Limitus – This is a deformity of the great toe joint that limits range of motion of the great toe joint. As the joint starts to reduce its motion this may also interfere with the normal gliding of the sesamoid bones and produce pain.
- Overuse- This may be the most common cause and typically develops gradually. This is especially true in activities that may cause a lot of weight bearing beneath the big toe such as ballet, dancing, basketball and volleyball to name a few.
- Shoe gear – If you wear high heels excessively it may cause sesamoiditis. Soft soled shoes would be best.
How is sesamoiditis diagnosed?
- Physical examination – your podiatrist will evaluate your foot to see if you have pain and swelling where the sesamoid bones are located.
- x-rays- these will be taken to see if the sesamoid bones appear normal.
- Congenitally abnormal – you may have been born with an enlarged sesamoid or one that is bipartite, has two parts. These abnormal presentations make it more likely to have pain from these sesamoids.
- Alignment – are the sesamoids positioned where they should be beneath the great toe joint. A bunion deformity will cause them to be misaligned and more likely to hurt.
- Fracture – the x-rays will also help to rule out a fracture.
How can I avoid sesamoiditis pain?
- Surgery – Surgery to remove the pain of damaged sesamoid may also be performed but only after conservative measured have failed. When surgery is performed it is usually the medial sesamoid that tends to be more prone to pain. This sesamoid is the one that is located towards the other foot.
- Reduce or eliminate activities – for some it may be practical to eliminate an activity that causes more stress to this area of the foot. For others better management of how much of the specific activity that is more likely to cause an injury should be considered. You should gradually increase each activity or consider doing it less frequently.
- Avoid high heels – these will tend to put more weight on the bottom of the great toe joint.
What is the Best Surgical and Non-Surgical Sesamoiditis Treatment?
Non-Surgical Treatments
- Rest and Activity Modification – Reducing weight-bearing activities to allow the sesamoid bones to heal.
- Orthotics – Custom orthotic inserts have been shown to have great success by limiting the amount of weight placed on the sesamoid bone to relieve pressure on the sesamoid bones.
- Padding and Taping – Protects the sesamoid bones and restricts excessive movement. This may help by minimaxing the motion in the joint and thereby reducing the pain.
- Cam-walker (short leg fracture brace) – By resting and limiting the motion of great toe joint.
- Anti-inflammatory NSAIDs and Ice Therapy – Helps reduce pain and inflammation in more acute stages where the pain has been short-term and not too severe. Using an Ice pack or wrapped may also help.
- Physical Therapy – Techniques like ultrasound and laser therapy to promote healing by reducing inflammation. We use the MLS (Multiwave Locked System) to accelerate healing.
- Corticosteroid Injections – May be used to reduce severe inflammation and pain. When combined with orthotics it has been shown to beeffective.
Surgical Treatments
- Sesamoidectomy – Removal of the affected sesamoid bone if chronic pain persists despite conservative treatments.
- Bone Drilling or Grafting – In cases of fractures, drilling may stimulate healing, while severe cases may require bone grafting.
- Joint Realignment Surgery – If misalignment from a bunion or hallux limitus contributes to pain, realignment surgery may be needed.
Finally, the number one way to reduce the chances of getting sesamoiditis and prevent recurrence
Orthotics you can have your cake and eat it too. The use of custom-made arch supports may be your best option as a sesamoiditis treatment. Especially if you want to do activities that might make you more prone to injury of the sesamoids. These activities may be tennis, pickleball, running, walking, basketball etc. With every step you take you reduce the load on the sesamoid bones. So don’t assume that you’ll always need to limit your activities or stop doing what you’re presently doing.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.
Frequently Asked Questions (FAQs) About Sesamoiditis
- What is the best sesamoiditis treatment?
The best treatment depends on severity. Non-surgical options like orthotics, physical therapy, and NSAIDs work well for most cases. Surgery is reserved for persistent pain or fractures. - How long does sesamoiditis take to heal?
Mild cases can heal within a few weeks with rest and treatment. More severe cases or fractures may take months. - Can sesamoiditis go away on its own?
If caught early and managed with proper footwear and rest, symptoms may subside. However, untreated cases can worsen over time. - When is surgery necessary for sesamoiditis?
Surgery is considered when conservative treatments fail, there is a chronic fracture, or the sesamoid bone is severely damaged. - Can I walk with sesamoiditis?
Walking is possible, but excessive pressure on the forefoot can worsen symptoms. Using orthotics or a walking boot can help reduce strain. - Does cortisone help sesamoiditis?
Cortisone injections can temporarily reduce inflammation and pain, but they are not a long-term cure. - What shoes should I wear for sesamoiditis?
Low-heeled, cushioned shoes with a wide toe box help reduce stress on the sesamoid bones.





 Soft tissue foot reconstructive surgeries may include treatment for ganglions and fibromas. Ganglions can originate from a tendon sheath or from joint capsule. In some cases, the doctor may be able to aspirate the fluid out with a needle in an office setting but if the problem returns or the ganglion is large surgical excision may be the treatment of choice. This can help with the pain and cosmetically improve the look of the foot or ankle.
Soft tissue foot reconstructive surgeries may include treatment for ganglions and fibromas. Ganglions can originate from a tendon sheath or from joint capsule. In some cases, the doctor may be able to aspirate the fluid out with a needle in an office setting but if the problem returns or the ganglion is large surgical excision may be the treatment of choice. This can help with the pain and cosmetically improve the look of the foot or ankle.