A strained muscle in the leg can happen suddenly during physical activity or build up over time with repetitive use. Whether it’s a mild strain from jogging or a more serious injury while playing sports, knowing how to recognize, treat, and prevent muscle strains is critical for maintaining mobility and avoiding long-term issues. In this blog, we’ll discuss the risk of muscle strains, risk factors, how to reduce swelling, and effective treatments to promote healing and prevent future injuries.
What Happens When a Muscle Strain Occurs in Your Leg?
A muscle strain occurs when the muscle fibers are stretched beyond their limit or even torn. You might feel a pop or sudden sharp pain when the injury happens. This is often accompanied by immediate weakness in the injured area, making it difficult to continue activity. Sometimes, the strain is mild and causes minor discomfort, while other times it can be a complete muscle tear, known as a grade three strain.
Recognizing the Severity of a Muscle Strain In The Leg
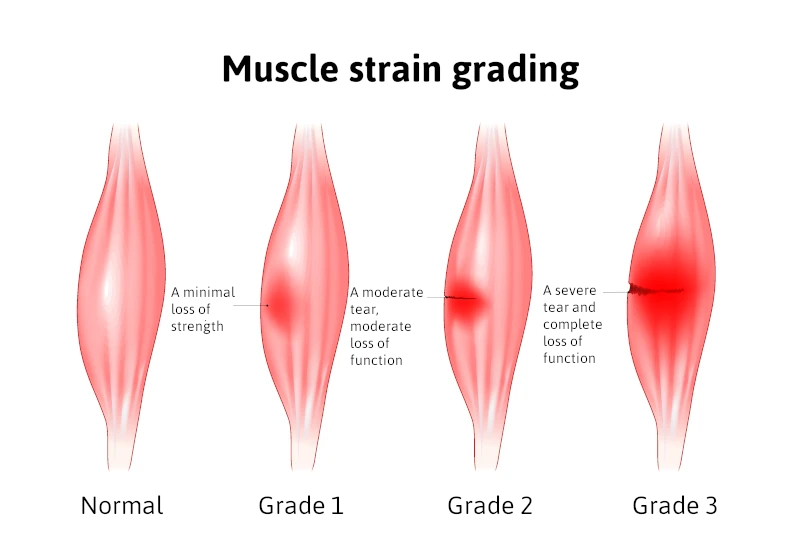
Strains are typically classified into three grades:
- Mild strain (Grade I): Minor damage to muscle fibers with little loss of strength or motion.
- Moderate strain (Grade II): More significant injury with noticeable weakness, swelling, and restricted movement.
- Severe strain (Grade III): Complete rupture of the muscle, often causing intense pain and the inability to use the affected leg.
In some cases, ongoing issues can lead to a chronic muscle strain, where the muscle has not fully healed and continues to cause discomfort during physical activities.
Risk Factors for Muscle Strains
Certain factors increase your risk of muscle strains, including:
- Inadequate warm-up before exercise
- Poor flexibility
- Muscle fatigue
- Previous muscle injuries
- Age-related changes to muscle elasticity
- Participation in high-intensity sports
Understanding these risk factors can help you take steps to protect yourself during activities.
How to Prevent a Muscle Strain in the Leg
Fortunately, you can take proactive steps to prevent muscle strains. Some of the best strategies include:
- Proper warm-up and stretching before exercise
- Strengthening exercises to support vulnerable muscles
- Staying hydrated and maintaining electrolyte balance
- Cross-training to avoid overuse of specific muscle groups
- Gradually increasing the intensity of your workouts
Consistency in these practices can significantly lower the chance that a pulled muscle will sideline you.
Immediate Treatment: Rest, Ice, Compression, and Elevation
When a strain occurs, early treatment is crucial for minimizing damage and speeding recovery. Follow the Rest, Ice, Compression, and Elevation (RICE) method:
- Rest the injured area immediately to prevent further muscle tearing.
- Apply ice wrapped in a cloth for about twenty minutes every two to three hours to reduce swelling.
- Use an elastic bandage for compression to limit inflammation.
- Elevate the leg above heart level whenever possible to decrease swelling.
These steps are essential within the first 48 hours after the injury.
Medications That Can Help
To manage pain and inflammation, doctors often recommend non-steroidal anti-inflammatory drugs such as ibuprofen. These medications work to reduce both pain and swelling. However, it’s important to use anti-inflammatory medications as directed and not rely on them as a substitute for proper rest and rehabilitation.
Rehabilitation: Regaining Strength and Flexibility
After the initial swelling and pain subside, it’s important to begin gentle rehabilitation exercises. Restoring range of motion without causing additional injury is the goal. Activities might start with light stretching, followed by progressive strengthening exercises. Physical therapy is often beneficial, particularly for moderate to severe strains.
Ignoring a muscle strain or returning to activity too soon can prolong recovery and increase the risk of chronic muscle strain. Taking the time to fully heal ensures the best long-term outcomes.
When to See a Doctor for a Muscle Strain in Leg
Most mild to moderate strains heal well with home care, but there are times when professional medical attention is necessary. Seek help if you experience:
- Severe pain and swelling
- Inability to walk or bear weight
- Numbness or tingling
- Noticeable muscle deformity
These symptoms could indicate a grade three strain or another serious injury that might require more advanced interventions, such as imaging studies or even surgery.
Long-Term Outlook
With prompt and proper care, most people fully recover from a leg muscle strain and return to their normal activities. Severe cases may take several months, while mild strains often heal within a few weeks. Adhering to treatment recommendations and rehabilitation plans is essential for preventing a recurrence. Once healed, it’s wise to incorporate injury prevention strategies into your daily routine. This not only minimizes the risk of muscle strains in the future but also helps enhance overall performance during physical activity.
Conclusion
A strained muscle leg injury can be frustrating, but understanding the injury process and knowing how to respond makes a huge difference in recovery. Remember that the risk of strains is higher if you have certain risk factors, but proper preparation and caution can prevent muscle strains. Treat early with rest, ice, compression, and elevation, and support healing with anti-inflammatory medications like ibuprofen when appropriate. Always listen to your body — if you feel a pop or experience intense pain, take it seriously. Healing takes time, but with patience, you can fully recover and return to your favorite activities stronger than ever.
Schedule Your Comprehensive Foot Evaluation Today
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.
With convenient clinical foot locations in Broomfield and Fort Collins, Colorado.