Many have heard of sciatic foot pain a term that refers to pain caused by the sciatic nerve. It’s been assumed that if you have nerve pain that radiates down your upper leg down into your lower leg and into the foot it’s likely sciatic pain. These sciatic symptoms will consist of nerve pain such as burning, tingling, and numbness that extends down to the foot causing foot pain. In many situations this may be, however, the purpose of this blog is to challenge this long-standing assumption. Yes, there may be another cause so treatment of your back with the eventual possibility of back surgery needs to be reevaluated as it may not always be the primary cause. Before we dive into this let’s make sure you have some basic understanding of sciatic foot pain.
Sciatic Foot Pain – The Conventional Approach
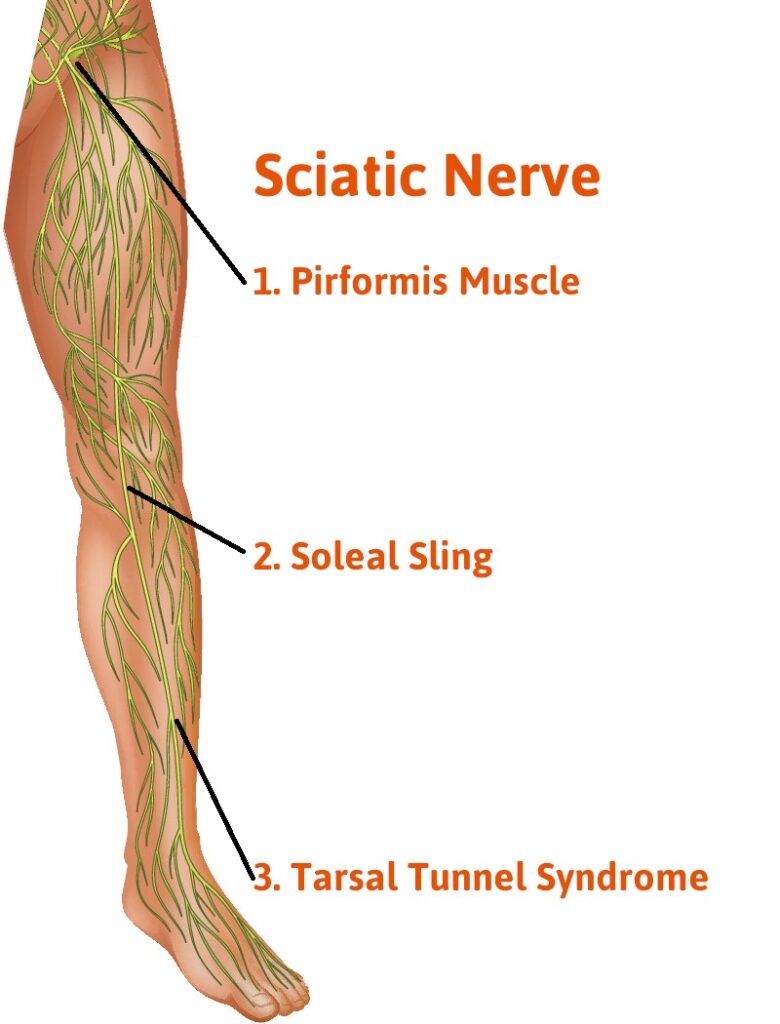
The sciatic nerve is the primary nerve that originates from the lower back. The origin is from nerve branches that originate from lumbar 1 and 2 and also sacrum 1,2,3. These branches form the sciatic nerve. There may be a herniated disk at one or more of these levels that creates sciatic pain from the nerve damage. Others may also have spinal stenosis at one of these levels or bone spurs causing pressure on the nerves.
Therefore conventionally the primary cause has always been that sciatic pain comes from pressure on the sciatic nerve as it originates from these branches. Following the nerve down into the leg it then travels down the buttock area into the back of the upper leg in the hamstring area. Just above the knee, it splits into two branches one is called the tibial nerve which travels down the back of the lower leg and eventually supplies all the nerves for the bottom of the foot. The other nerve called the common peroneal nerve travels to the outside of the knee just below the knee joint. It eventually supplies the majority of the top of the foot.
As we already mentioned this is the primary nerve that supplies nerves to the top of the foot. It’s important to note that right after it splits off from the sciatic nerve just above the knee joint and travels around the outside of the knee it goes through a nerve tunnel. This nerve tunnel is referred to as the common peroneal nerve tunnel. It’s very similar to the ulnar nerve tunnel of the elbow which patients may be more familiar with. For over two decades, I have been doing decompression surgeries on this nerve tunnel to open it and relieve pressure on the common peroneal nerve.
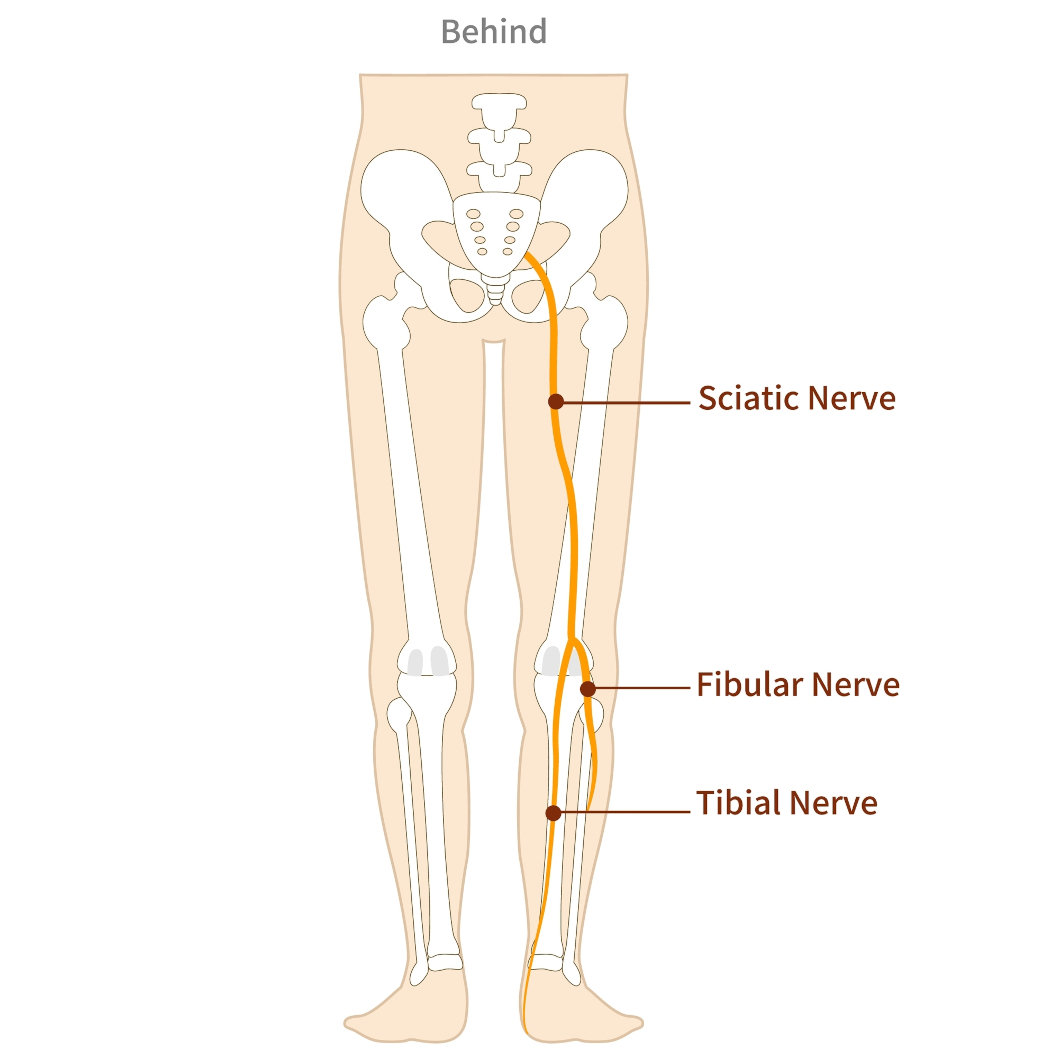
The common peroneal nerve can be implicated nerve conditions such as neuropathy, restless legs syndrome, and drop foot. I have been able to reverse each of these conditions by doing surgery on this nerve tunnel. Read my paper on Common Peroneal Nerve. We have also discovered that some of these patients suffering from neuropathy, restless legs, or drop foot may also be experiencing sciatica foot pain. They report nerve symptoms in the buttock area going down into the upper leg that disappear when we decompress the common peroneal nerve.
Double Crush Syndrome
A simple definition of double crush syndrome is when a peripheral nerve has one area of compression on the nerve, but another area of compression may also exist. Therefore we call it double crush . The interesting thing about this concept is that these two areas of compression affect each other. In other words, using sciatica as an example a bulging disc or bone spur may be creating compression on the peripheral nerves as they exit the spinal cord in the back and further down the leg at the location of the common peroneal nerve tunnel there is also compression sciatic pain can be reversed without back surgery. Why? By eliminating pressure on the common peroneal nerve at its tight nerve tunnel compression will still exist in the back but the sciatic nerve will be less sensitive to the compression and sciatic nerve pain will be reversed.
That is why in my many years of doing surgery on the common peroneal nerve we have noted that patients may have pain relief above the knee along the sciatic nerve into the back and also below the knee into the foot. Again there is still compression in the back that may be observed with an MRI however the nerve at the location is less sensitive and therefore the sciatic symptoms are not only relieved above the knee going into the back but also from the knee going down into the foot.
What is the significance of Double Crush and Common Peroneal Nerve Entrapment?
- Avoiding back surgery – It could be that back surgery could be avoided as the common peroneal nerve is playing a larger role that was ever understood. Decompression of the common peroneal nerve would be less risky.
- Failed back surgery – When back surgery has failed to eliminate sciatic pain or back pain decompression of the common peroneal nerve may be involved and offer another option rather than a repeated back surgery attempt.
How do we know if the Common Peroneal Nerve is an Issue?
- Clinical examination – Patients may have slight muscle weakness, drop foot, and loss of sensation along the distribution of the common peroneal nerve. Symptoms may be present on the top of the foot and the front of the leg.
- Diagnostic ultrasound – Imaging by using ultrasound may show compression at the nerve tunnel.
- Emg and nerve conduction studies – These studies can sometimes show the involvement of the common peroneal nerve but are not always highly accurate.
- Diagnostic injections – a new technique called the Phoenix test can be used. This involves using a small amount of local anesthesia and placing it under the skin but above the common peroneal nerve. Ultrasound guidance is used for precise placement of the anesthesia. Within minutes patients will usually respond resulting in dramatic symptom relief which will help support that the common peroneal nerve tunnel may be the root cause of the symptoms.
So if you’re trying to get relief from your sciatic foot pain that is extending into your foot it is important the consider the possibility of the common peroneal nerve being an issue. Please understand that unless you are seen by a peripheral nerve surgeon this possibly may not be a consideration.
Schedule your appointment online or call our Fort Collins and Broomfield, Colorado locations to connect with a trusted foot doctor near you at our renowned foot and ankle clinic.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.
References
Maejima R, Aoyama M, Hara M, Miyachi S. Double Crush Syndrome of the Lower Limb in L5 Radiculopathy and Peroneal Neuropathy: A Case Report. NMC Case Rep J. 2021 Dec 22;8(1):851-855. doi: 10.2176/nmccrj.cr.2021-0169. PMID: 35079559; PMCID: PMC8769459.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8769459/