One of the most common foot and ankle complaints I see in my patients is pain in the ball of their foot. The feeling of your sock wrinkled, or something in your shoe? Maybe an uncommon burning or tingling in your toes? You could have experienced an increased pain while in your tight shoes, high heels, or ski boots? These are the stories we hear from those suffering from Morton’s Neuroma.
What is a Neuroma?
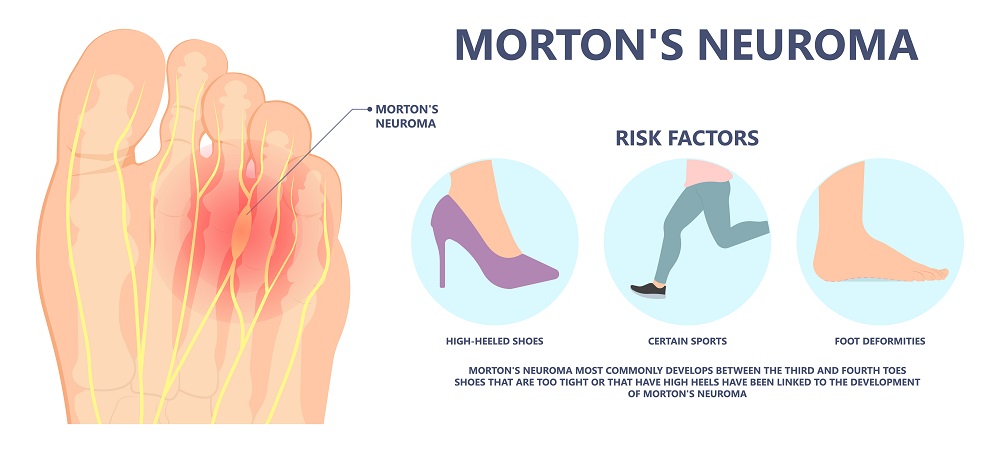
The foot is built with a ligament that runs across the ball of the foot which we bear weight upon. This is called the transverse metatarsal ligament. Between the ligament and skin on the bottom of your foot is where the problem starts. It is thought that the ligament can rub on the nerve which irritates it. The nerve may even become swollen, which is what causes that “full” feeling so many people describe. Neuromas most frequently occur between the third and fourth toe called a Morton’s neuroma, or between the second and third toes. The word neuroma may imply a tumor, but it is not. No need to fear, the nerve is simply swollen from the pressure of the ligament.
What Causes a Neuroma?
Neuromas may just happen! There is no correlation with certain foot types. There may be little evidence to suggest that flatfeet or high arch feet are problematic. However, one exception is called Morton’s Foot. This is a foot that has a short first metatarsal bone that is the bone for the great toe joint. When it is too short, it places more weight on the second or third interspaces.
Additional Causes
- High Heel Shoes: These put more weight on the ball of the foot.
- Tight Fitting Shoes: This may squeeze the metatarsal bones on the foot on the nerve and injure it.
- Trauma: When something is dropped on the foot, or the toes are extended upward in the case of stubbing your toe.
- Bunions: Having a bunion deformity will make your foot wider, and this can make shoes tighter causing a neuroma.
How Do You Know If Your Foot Pain is From Morton’s Neuroma?
- X-rays: Taking x-rays can rule out other bone or joint problems that can mimic a neuroma. But a neuroma cannot be seen on x-ray, as it is a soft tissue problem.
- Ultrasound: Using ultrasound imaging can often show that the nerve is swollen
- MRI: This form of imaging may also be useful.
Out of all, the most important step to knowing is a doctor’s clinical examination and your specific symptoms.
When it comes to treatment, you may find relief by doing the following: Avoid wearing shoes that are too tight, and wear shoes that have plenty of width. Avoid high heels, as this puts more weight on the ball of the foot. Use ice packs, especially in the early stages. Try over the counter shoe inserts.
If these options fail for Morton’s Neuroma, the options that your podiatrist would consider could be:
- Cortisone Injections: A series of two or three of these may resolve the pain permanently
- Custom Shoe Inserts: This can be highly successful as they get to the root cause of the problem. This treats the source by supporting the bony structures and ligaments so irritation to the nerve is reduced. The orthotics are made from a non-weight bearing neutral position of your foot to optimize support and control.
- Laser Treatment: Lasers may also be very successful. It works on the concept of helping the mitochondria in your nerve cells. In every cell of your body, there is an area called the mitochondria that creates energy for the cell. Laser helps the cells to repair.
- Regenerative Medicine: We have had success with regenerative medicine (stem cell). This shows some promise for neuroma pain that is not severe after other conservative treatments failed.
Two Surgical Options for Morton’s Neuroma
- Nerve Decompression Surgery: The surgeon will make an incision on the top of the foot and release (decompress) the ligament above the nerve, so it no longer irritates the nerve.
- Nerve Resection: When this surgery is performed, not only does the surgery cut the ligament to get access to the nerve, but also then removes a section of the nerve
Pros and Cons of These Two Options
This surgeon prefers the nerve decompression technique because of its high success rate, and you’re keeping your nerve. The foot tends to feel more normal after this surgery than if the nerve branch is removed. When nerve resection is performed, the foot may not feel as normal but also the nerve stump that is left behind can cause another issue called “amputation neuroma” or “nerve stump”. This can cause another issue for the patient. Along with this, the Associations of Extremity Nerve surgeons who arguably are the best trained doctors for lower extremity nerve evaluation and treatment, support nerve decompression and advise against neuroma resection.
Nerve Ablation and Alcohol Injections: These options are less common amongst podiatrists. The drawback to both options is that they are destructive to the nerve. Alcohol injections gradually kill the nerve over a series of injections. Nerve ablation uses heat to kill the nerve. If alcohol injections or nerve ablation fail, then it makes the option of nerve decompression less optimal as the nerve has been damaged, and nerve section will more likely be suggested by the surgeon. That’s why this surgeon does not suggest these treatments as my philosophy is to keep the nerve.
When either of these surgeries is performed, the patient may walk immediately, and most patients are back to regular shoes in 3 weeks. The good news is that many patients we see can avoid surgery. Early treatment is important. If you take the steps we’ve discussed and the pain persists, make sure to contact your podiatrist.





