Ankle sprains are the most common injury in the foot and ankle. In this blog, we will discuss the two types of ankle sprains. The most common type is a low ankle sprain and a sprain that occurs less frequently is referred to as a syndesmotic ankle sprain or high ankle sprain. You will learn how both these injuries can occur and gain insight into determining if you have such a sprain.
The Basics
Before categorizing a high ankle sprain versus a low ankle sprain, we must first understand the anatomy. The ankle joint is formed by the talus which sits between the two leg bones called the tibial bone and the fibula bone. The fibula is a smaller bone that lies on the outside of the leg and opposite of the other leg.
Low Ankle Sprains
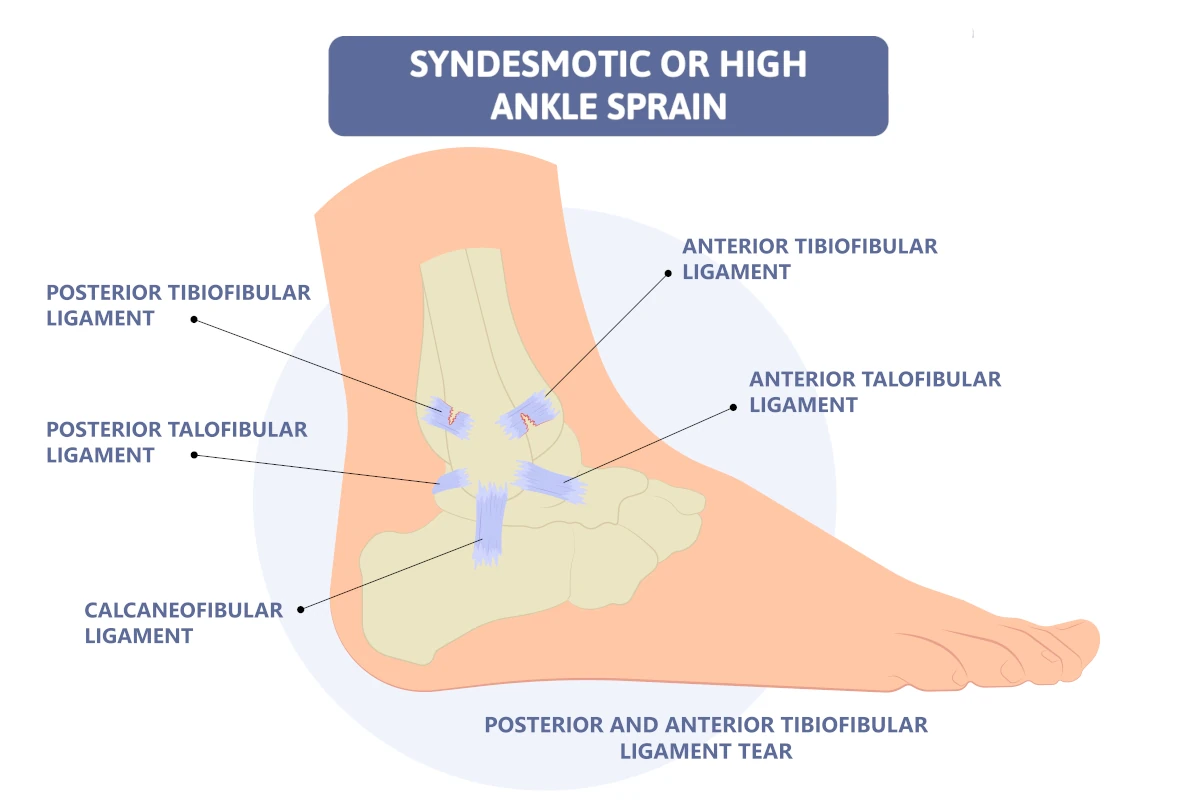
When you have a low ankle sprain, it involves the ligaments that attach the end of the fibula bone on the outside of your ankle and the end of the tibial bone in the inside of your ankle to your foot. There is one major ligament on the inside that connects the tibia to the foot which is called the deltoid ligament. There are three ligaments on the outside of the ankle connecting the fibula to the heel (calcaneus) and the talus bone. These are called the anterior talofibular ligament, calcaneofibular ligament, and posterior talofibular ligament. These ligaments are all involved in low ankle sprains.
High Ankle Sprains
The other ligaments that are referred to as high ankle ligaments support the ankle joint structure are less frequently injured and they connect the leg bones, tibia and fibula, together. When these are injured, it is referred to as a syndesmotic ankle sprain. They are called the anterior and inferior tibiofibular ligament, posterior and inferior tibiofibular ligament, inferior transverse ligament, and the interosseus membrane.
- Anterior and inferior tibiofibular ligament – this ligament is towards the front of the leg just above the ankle and connects the larger tibia bone to the smaller fibula bone.
- Posterior and inferior tibiofibular ligament – this ligament connects the back portion of the larger tibia bone to the smaller fibula bone.
- Interosseous membrane – this fibrous membrane lies between the two ligaments and its function is to connect the tibia and fibula together.
- Inferior transverse ligament – it goes on the back of the ankle, and it goes from the fibula to the tibia, and it is closer to the ankle ligament.
How does a high ankle sprain occur?
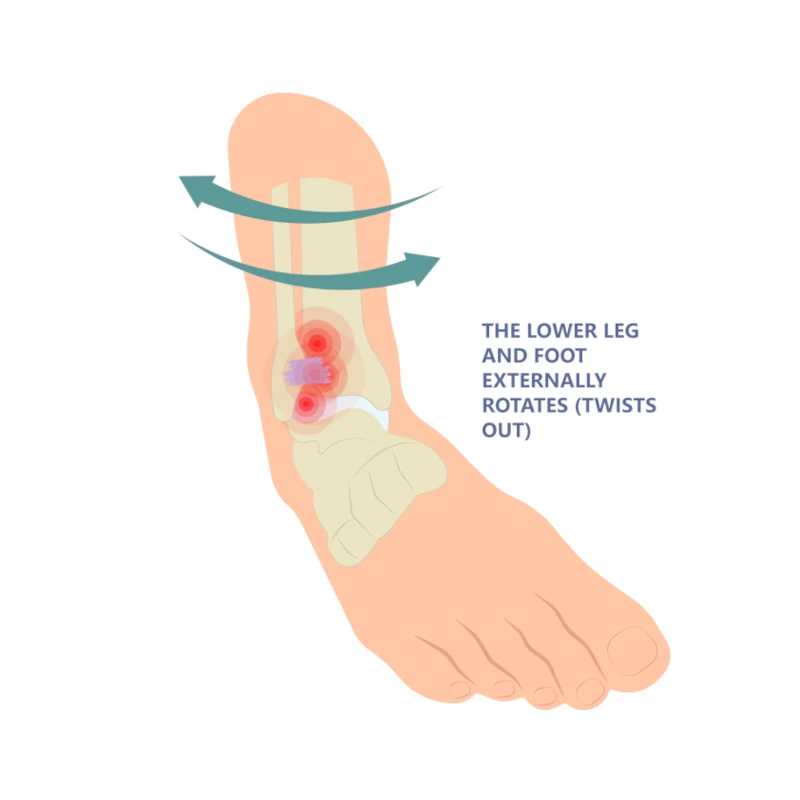
High ankle sprain occurs typically when the foot is flexed upwards, and the foot is planted on the ground and there is significant twisting of the leg around the ankle joint most commonly with external rotation. This can put stress on the bones and partially or fully tear the ligaments that are higher above the ankle joint. In contrast, the low ankle sprains are much more frequent with the foot being typically in a downward position, and the foot will rotate inward or outward in relationship to the leg. Syndesmotic ankle sprains occur more frequently in activities such as football where the foot is planted on the ground and possibly because of a collision, twisting is occurring in the leg.
How do I know if I have a high ankle sprain?
Typically, a high ankle sprain will not present with a significant swelling in the outside or inside of the ankle or foot, but pain will be above the ankle joint. You will have swelling in the lower leg region. And also, you may have had the injury when your foot was planted firmly on the ground and the foot was flexed upward.
How is a syndesmotic ankle sprain diagnosed?
The doctor will inquire about how the injury occurred. The examination will usually show pain and swelling in the lower leg close to the ankle and the doctor will perform a squeeze test where the tibia and fibula bones are squeezed together, and this will typically create pain.
X-rays
X-rays will be taken, and, in some cases, there will be a fracture noted particularly in the fibula bone or there could be a portion of bone that was pulled away by one of the injured ligaments. If there appears to be a separation between the tibia and fibula bone on x-ray, surgery may be needed to bring the two bones back into a more anatomical alignment.
CAT scans
CAT scans may be useful to more specifically evaluate for possible bone injury to the tibia and fibula and to ensure that no fracture is associated with syndesmotic injury.
Treatment for a syndesmotic ankle sprain
- Rest, Ice, and Compression – if the injury is milder, cutting back on activities and resting the area, icing, and wrapping it with compression is helpful. Anti-inflammatory may be used
- Physical Therapy – physical therapy may be needed to reduce the swelling and promote returning to full activity.
- Immobilization – in more severe cases, it may be recommended not to bear weight on the ankle for a period of time or simply wear a CAM walker as part of the recovery.
- Surgery – if there is any fracture where displacement may be present or an injury was severe enough to cause more separation between the tibia and fibula bone, surgery may be suggested.
Because ankle sprains are one of the most common injuries of the lower extremity, it is important to understand the concept that they are frequently under-evaluated and under-treated. For many, treatment of an ankle sprain may involve a visit to an urgent care facility, nothing shows up on an x-ray and they are advised to use an ace wrap, ice the area and gradually return to regular activity.
It is important to consider getting a consultation with a foot and ankle specialist to make sure you get an accurate diagnosis, and that appropriate treatment is done early so that you may get back to full activity sooner with less ankle complications in the future. Finally, syndesmotic ankle sprains are a rare occurrence but important for you to know about so that if you suspect you have one, you can seek a consultation with a foot and ankle specialist.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.



 Secondly, do you have a condition that continues to plague you in spite of attempts with anti-inflammatories, icing, resting or maybe even physical therapy? Do you find that if you lay off from running or walking and return to it, the same problem occurs? If this is you, then this blog is right for you! Let’s find out if custom orthotics for foot problems are right for you.
Secondly, do you have a condition that continues to plague you in spite of attempts with anti-inflammatories, icing, resting or maybe even physical therapy? Do you find that if you lay off from running or walking and return to it, the same problem occurs? If this is you, then this blog is right for you! Let’s find out if custom orthotics for foot problems are right for you.