Plantar plate tear is not a common foot and ankle complaint, and it can be challenging to diagnose. Understanding the symptoms and causes of this foot issue is crucial for those experiencing severe pain and swelling in the ball of the foot, particularly around the second toe. In many cases, there is no history of injury, making early diagnosis even more essential. This blog explores the complexities of the plantar plate, its common causes, symptoms, diagnosis, and treatment options.
What is the plantar plate?
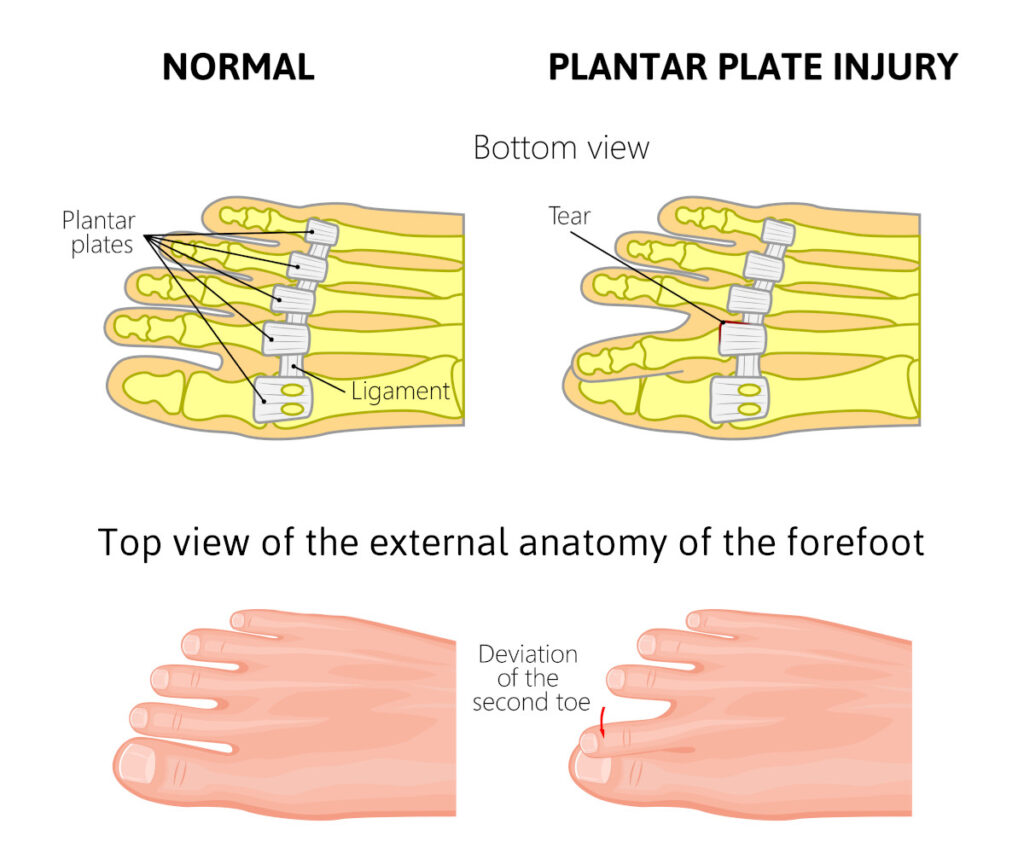
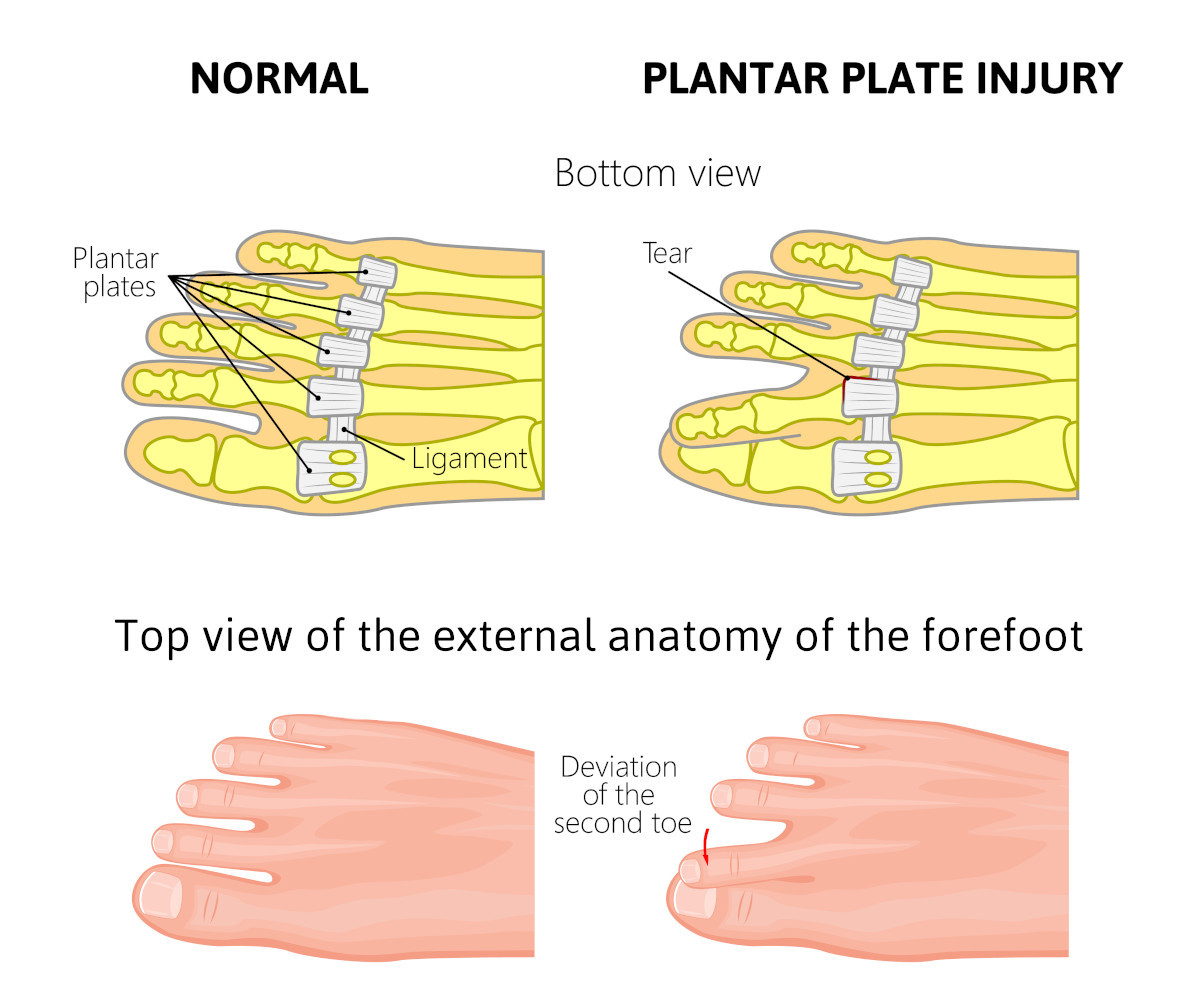
The plantar plate is a ligamentous structure that spans the ball of the foot. It connects the metatarsal heads, those areas of the foot we rely on for support, and helps prevent them from spreading apart. Additionally, it acts as a safeguard for the weight-bearing area in the ball of the foot, making it a vital part of foot anatomy. Its role in maintaining foot health is rather intricate.
What causes a plantar plate tear?
Several factors can lead to a tear:
- Long Second Metatarsal Bone (Morton’s Foot): A long second metatarsal bone can create excessive weight on the second metatarsal phalangeal joint, leading to added stress on the plantar plate and resulting in a tear.
- Over-Pronation: Excessive flattening of the foot, also known as pronation, can place undue weight on the joint, potentially causing a tear in your plantar plate.
- Bunions: Bunions, the enlargement of the base of the big toe, can increase the width of the foot, contributing to stress on the plantar plate.
- Activities: High-impact activities like running, climbing stairs, and dancing can place an increased load on the ball of the foot, making it more susceptible to plantar plate injuries.
Symptoms of a tear to the Plantar Plate
Identifying a ear typically involves the following symptoms:
- Swelling around the second toe joint in the ball of the foot.
- Deviation of the second toe toward the first toe.
- Pain when moving the second toe joint.
- Spreading of the lesser toes, especially the second and third toes.
Diagnosing a tear involves a combination of patient presentation and medical imaging:
- A physical examination, which may give the doctor reason to suspect a tear of the plantar plate.
- X-rays to rule out bone or joint problems.
- MRI scans to evaluate the soft tissue structures around the joint for potential damage.
Management of a tear to the plantar plate
In the early stages of a plantar plate tear conservative measures can be effective:
- Resting the affected area and applying ice to the affected toe may help.
- Taping the second toe in a more correct position toward the third toe can relieve stress on ligaments.
- Anti-inflammatories can alleviate pain.
- Physical therapy can be beneficial, especially if symptoms are not severe.
Treatment by a Foot Specialist
For more specialized care, consult a foot specialist. Depending on the severity of the condition, here are treatment options:
- Splinting with Tape: In the early stages, instructions on how to splint your toe with tape may be helpful.
- Custom-Made Orthotics: For those with overpronation, custom-made orthotics can provide the necessary support.
- Surgery: If conservative measures fail, surgery may be suggested, with various approaches available. Surgery may involve repairing the tear, repositioning tendons around the joint, or removing a portion of the joint, depending on the specific circumstances. The severity of the condition and your foot type determine the surgical approach.
- Recovery from Surgery: Recovery times vary depending on the surgical method, ranging from several weeks to 3-4 months, with weight-bearing often allowed soon after the procedure.
If you or someone you know is experiencing symptoms that suggest a plantar plate tear, it’s crucial not to delay seeking professional attention from a local podiatrist. Early treatment may prevent the need for surgery, but if surgery is necessary, it can be very successful. Don’t hesitate to address the issue and start your journey toward a pain-free and fully functioning foot.


 To begin, every patient we see with heel pain has an ultrasound examination of their heel. We know what the normal appearance of fascia should be by immense studies that have been performed. Generally, a patient with plantar fascia pain will have a thicker and darker appearing fascia in the area where it attaches to the heel bone. A diagnostic ultrasound is extremely useful to ensure that your pain is truly from fascia. If the fascia looks normal, we will then suspect the nerve problem.
To begin, every patient we see with heel pain has an ultrasound examination of their heel. We know what the normal appearance of fascia should be by immense studies that have been performed. Generally, a patient with plantar fascia pain will have a thicker and darker appearing fascia in the area where it attaches to the heel bone. A diagnostic ultrasound is extremely useful to ensure that your pain is truly from fascia. If the fascia looks normal, we will then suspect the nerve problem.










