Bunions are one of the most common foot deformities that cause terrible inconvenience to daily life. In this blog, we will share with you some conservative at-home treatments for bunion pain relief, before having to opt for surgery. Did you know bunions tend to be more common for women than men? Many people suffer because of wearing shoes that place pressure on the bunion bump. Although tight-fitting dress shoes have been thought to be a cause it is thought the be from other factors. Pregnancy because of increased ligamentous laxity and women may inherit the foot mechanics that lead to the problem. At our Fort Collins clinical location we have seen a number of patients with bunion issues and helped relieve their pain.
What is a bunion?
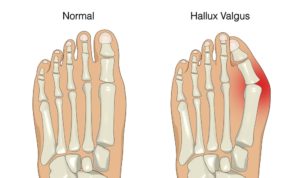
A bunion, also known as hallux abducto valgus, is the misalignment of the great toe. As part of the deformity, the great toe begins to deviate towards the second two, and this is followed by an increased enlargement of the first metatarsal at the base of the joint. The first metatarsal bone then starts to shift away from the second metatarsal bone, causing serious misalignment. This is responsible for most of the swelling in the big toe knuckle.
What causes bunions?
 It is a popular notion that shoe gear is the primary reason one develops a bunion. However, most foot specialists agree that improper foot mechanics from inherited foot type plays a larger role. In fact, it has been noted in some cultures such as tribes in Africa and New Guinea, that shoes are rarely worn, yet bunions are still present within the populations. You may hear, “My mom had bunions and now I do too!”, as a pretty common phrase that goes around.
It is a popular notion that shoe gear is the primary reason one develops a bunion. However, most foot specialists agree that improper foot mechanics from inherited foot type plays a larger role. In fact, it has been noted in some cultures such as tribes in Africa and New Guinea, that shoes are rarely worn, yet bunions are still present within the populations. You may hear, “My mom had bunions and now I do too!”, as a pretty common phrase that goes around.
Why do bunions hurt?
Misalignments will create a large prominence by the great toe joint, thus making the foot wider and more difficult to fit into shoes. The great toe may also rub against the second toe, causing severe and continuous pain.
Treatments for bunion pain: At-home remedies to try
- Wider shoes – You may consider getting wider shoes. Women may need to limit their styles and duration of time in dressy shoes. It is best to avoid pointed, narrow shoes, or high heels for long periods of time.
- Padding – Various pads can also be used inside the shoes to protect the bunion bump from rubbing the shoe.
- Toe splints – You may also try toe splints that straighten the toe when they are worn.
- Over-the-counter arch supports – These may support the great toe joint area and give some relief.
- Ibuprofen and icing –Using an ice pack or an anti-inflammatory medicine such as Ibuprofen may offer temporary relief from bunion discomfort. They assist in immediately reducing pain and inflammation.
What your podiatrist may do for bunion pain relief
Orthotics
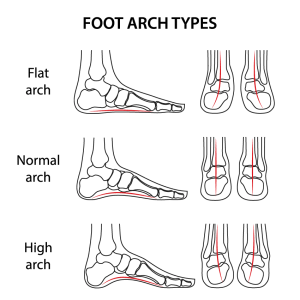
Many podiatrists will use orthotics on a conservative basis, especially if the bunion is in its early stage – as patients are more likely to get bunion pain relief this way. The orthotics can help stabilize and support the great toe joint and redistribute weight more evenly. They may also biomechanically slow down the progression of the deformity.
Podiatrists have training in biomechanics and believe in placing the foot in what is called its “neutral point non-weight bearing” position. This means we place the foot where it should be, not where it is when bearing weight. A digital scan is used to capture this foot position. The patient will get a very precisely made orthotic that will have the potential to provide maximum benefit.
Scanning of the foot to get a digital 3-D model of a patient’s foot at our Fort Collins and Broomfield clinic to address common foot problems like bunions.
Surgery
Failure after trying conservative treatments may need surgery for bunion pain relief. Surgery does have a high success rate and the recovery time can vary depending on the type of correction that is needed. One advantage of not waiting too long to have bunion correction surgery is that more severe bunions can require techniques that leave you non-weight bearing for a longer period of time. Most bunion surgeries, however, will allow you to be back in lace-up shoes in three to four weeks.
In most promising scenarios, patients are able to bear weight on the foot in the first week. Several surgical techniques we follow involve removal of the bony prominence and then shifting the first metatarsal bone that is out of alignment so that it is back in its original position. This corrects the deformity and narrows the foot making shoe selection easier.
Patient Testimonial Video of how Susan’s Bunions were fixed!
How to know if surgery is right for you?
The decision for surgery is a very personal one. Each patient may have different goals in their mind. You may want to discuss your options with our team of specialists before you pick your treatment plan. Our staff and podiatrists will be available should you need any assistance regarding your foot and ankle health.
Suffering from bunion pain is definitely not worth it and it is important to consider a consultation with our podiatrists to see what’s right for you.
by Dr. Anderson






 Soft tissue foot reconstructive surgeries may include treatment for ganglions and fibromas. Ganglions can originate from a tendon sheath or from joint capsule. In some cases, the doctor may be able to aspirate the fluid out with a needle in an office setting but if the problem returns or the ganglion is large surgical excision may be the treatment of choice. This can help with the pain and cosmetically improve the look of the foot or ankle.
Soft tissue foot reconstructive surgeries may include treatment for ganglions and fibromas. Ganglions can originate from a tendon sheath or from joint capsule. In some cases, the doctor may be able to aspirate the fluid out with a needle in an office setting but if the problem returns or the ganglion is large surgical excision may be the treatment of choice. This can help with the pain and cosmetically improve the look of the foot or ankle.