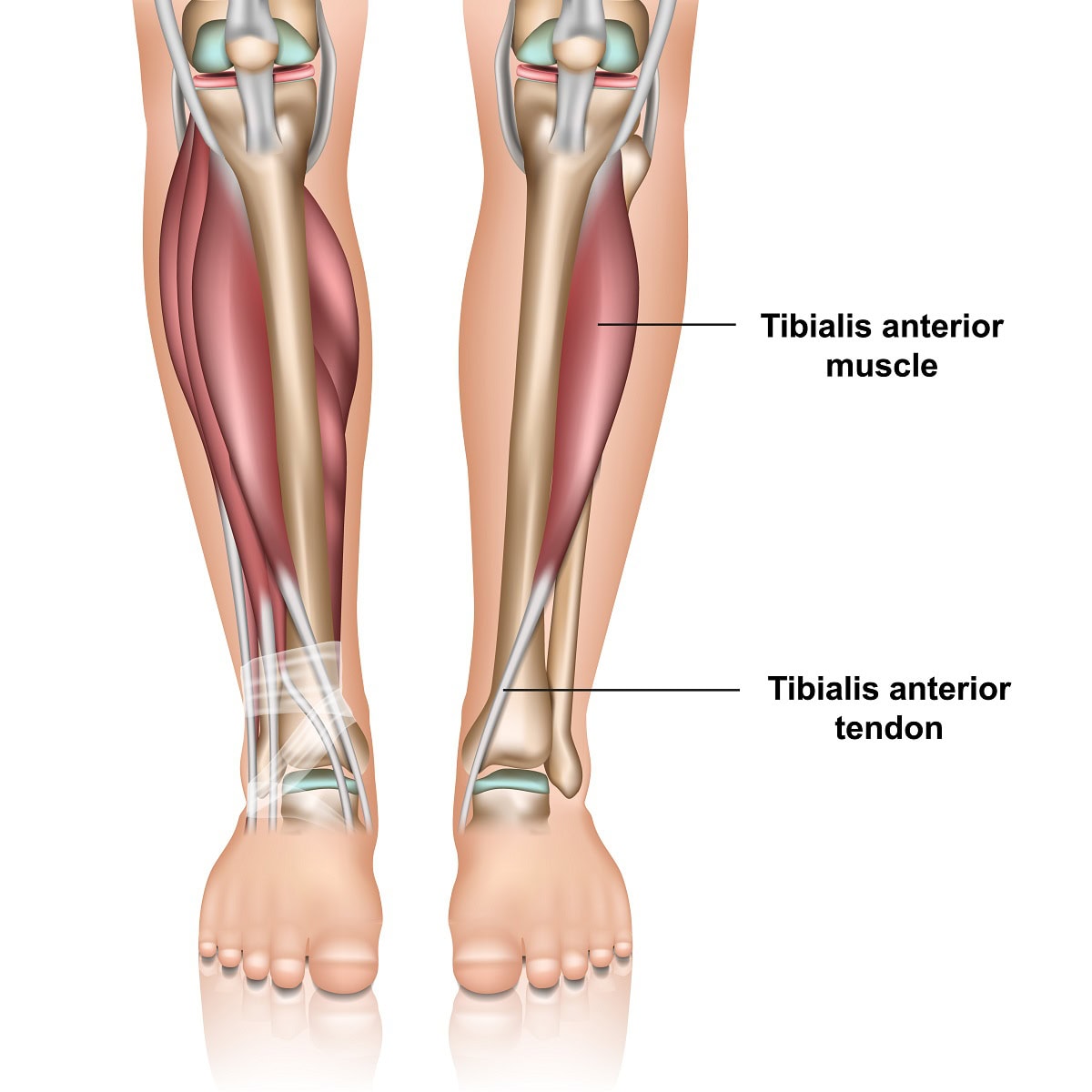
A person may experience tibialis anterior pain and not consider looking into what could be causing the issue. The tibialis anterior tendon is located in the lower leg along the shin bone, tibia. It is the third largest tendon going into the foot with the Achilles tendon being the largest and posterior tibial tendon the second largest. It’s function is to pull the foot up towards the knee. Without it your foot would slap down as you walk as the heel strikes the ground. It also helps to supinate your foot as it helps to support the arch. This tendon is important for normal gait as it is needed for your foot to clear the ground as you walk or run.
Where is anterior tibialis tendonitis pain located?
For the majority of patients, the pain will be above the ankle joint along the shin bone. It may also occur in front of the ankle and down into the foot where it inserts in the foot onto the navicular bone. This bone is halfway between the great toe joint and the ankle joint. It is less common to cause pain in the foot itself.
What causes tibialis anterior pain?
- Overuse – doing too much too soon can be a cause. Any activity that requires excessive use of the tibialis anterior muscle may be a cause. Because the tibialis anterior muscle is used to decelerate downward motion of the foot at the ankle joint and is used for pulling the foot upwards a the ankle joint motions that may amplify these motions may cause overuse. Example would be hiking on steep terrain as when walking downhill the muscle is used more to decerlate the downward motion of the foot so your foot doesn’t slap the ground. Racquet sports may also be more likely to cause excessive use of the muscle and tendon.
- Trauma – You may also have a full or partial rupture of the tendon from and ankle injury. This could be caused by a laceration to the tendon or by any force that places excessive downward motion on the foot.
- Foot types – certain foot types may be more likely to cause tibialis anterior tendonitis. Because the tendon helps to support the arch a flat foot is more likely to place excessive stress on the muscle and tendon.
- Foot drop – When there is a partial or full rupture of the tibialis anterior tendon a foot drop may develop. Because the primary function of the tendon is to move the foot upwards, if it loses its function the foot will slap against the ground when walking or running. This can lead to ankle sprains as it has a significant effect on balance and stability.
How is tibialis anterior pain diagnosed?
- Clinical examination– The doctor will find pain and swelling along the shin bone on the front of the leg adjacent to the tibia. Or there will be pain along the tendon in front of the ankle and down into the foot where the tendon attaches to the top of your arch. There may be pain when you pull the foot up in these same areas. If there is a partial or full tear of the tendon it may be difficult to pull the foot upwards.
- Diagnostic ultrasound– This is a imaging technique that can be used to access the integrity of tendon and muscle.
- MRI– The doctor may also use MRI which can very accurately evaluate a potential tear and he severity of it.
- Gait analysis – simply watching you walk may help to rule out foot drop which could be caused by a tibialis anterior tear.
Treatment options for tibialis anterior pain
- Rest and anti-inflammatories – this can be useful if the pain is not long term and the pain is mild.
- Immobilization – Using a Cam walker to walk in can also be helpful as it will help rest the tendon and muscle.
- Modification of activities – Choosing another activity or decreasing the activity that may have contributed to the problem may be recommended.
- Orthotic devices – Custom made arch supports may help to reduce the stress placed on the tendon as it may be overused in attempting to support the arch of the foot.
- Physical therapy – different physical therapy modalities may also be helpful.
- Laser treatment – Use of MLS laser for pain treatment has also been proven successful in our practice for tendonitis issues.
- Surgery – When a tear or partial tear is present surgery may be recommended to maintain the integrity of the tendon. This type of surgery may require non- weight bearing for minimum of 4 weeks.
Tendonitis versus tendinosis – We now know that what was once thought to be an inflammatory issue , tendonitis may be incorrect and in fact it’s more likely that the tendon is breaking down. There may be small microscopic tears in the tendon. This is often referred to as tibialis anterior tendonopathy. For close to two decades now we have had great success with the use of Human Cellular tissue products.
What are human cellular tissue products?
Sometimes referred as stem cell treatment this can alleviate the need for surgery. When there is severe pain along the tendon, and the MRI or ultrasound reveals tears this treatment can be used. This form of treatment has greatly reduced the need for the surgical repair of tendons in our practice. It is not suggested for a full tendon tear but when the tears are minor or partial it can work extremely well.
How would human cellular tissue products be used?
This is done in a clinic setting. The area where the tendon tear is located is numbed with local anesthesia so it’s a pain free experience. Then with the use of diagnostic ultrasound to locate the area of tendon damage the stem cell product is injected into the area. The patient is allowed to walk immediately and uses a Cam walker to walk in for four weeks.
So consider these options if you have tibialis anterior pain. And one last consideration is to avoid the use of cortisone in the area of the tendon. I do not consider this a good option as it can potentially weaken the tendon and perhaps cause a rupture.
Easily schedule your appointment online or contact our skilled foot doctors at the nearest foot and ankle clinic in Fort Collins or Broomfield, Colorado to find the best podiatrist near you.
Call us today at our Fort Collins location (970) 329-8158, Broomfield location (303) 997-2795, Surgery Center (970) 329-8158, or use our online scheduling system to book your appointment.